- Home
- »
- Specialties
- »
- Hepatology Billing Services
Hepatology Billing Services | Hepatology Medical Billing
Welcome to CLICKVISIONBPO, your trusted hepatology billing company.
We specialize in offering comprehensive gastroenterology hepatology medical billing services to help your practice streamline billing processes, reduce errors, and ensure timely payments.
With our expertise in hepatology billing services, you can focus on patient care while we handle the complexities of medical billing.
Our Hepatology Medical Billing Services
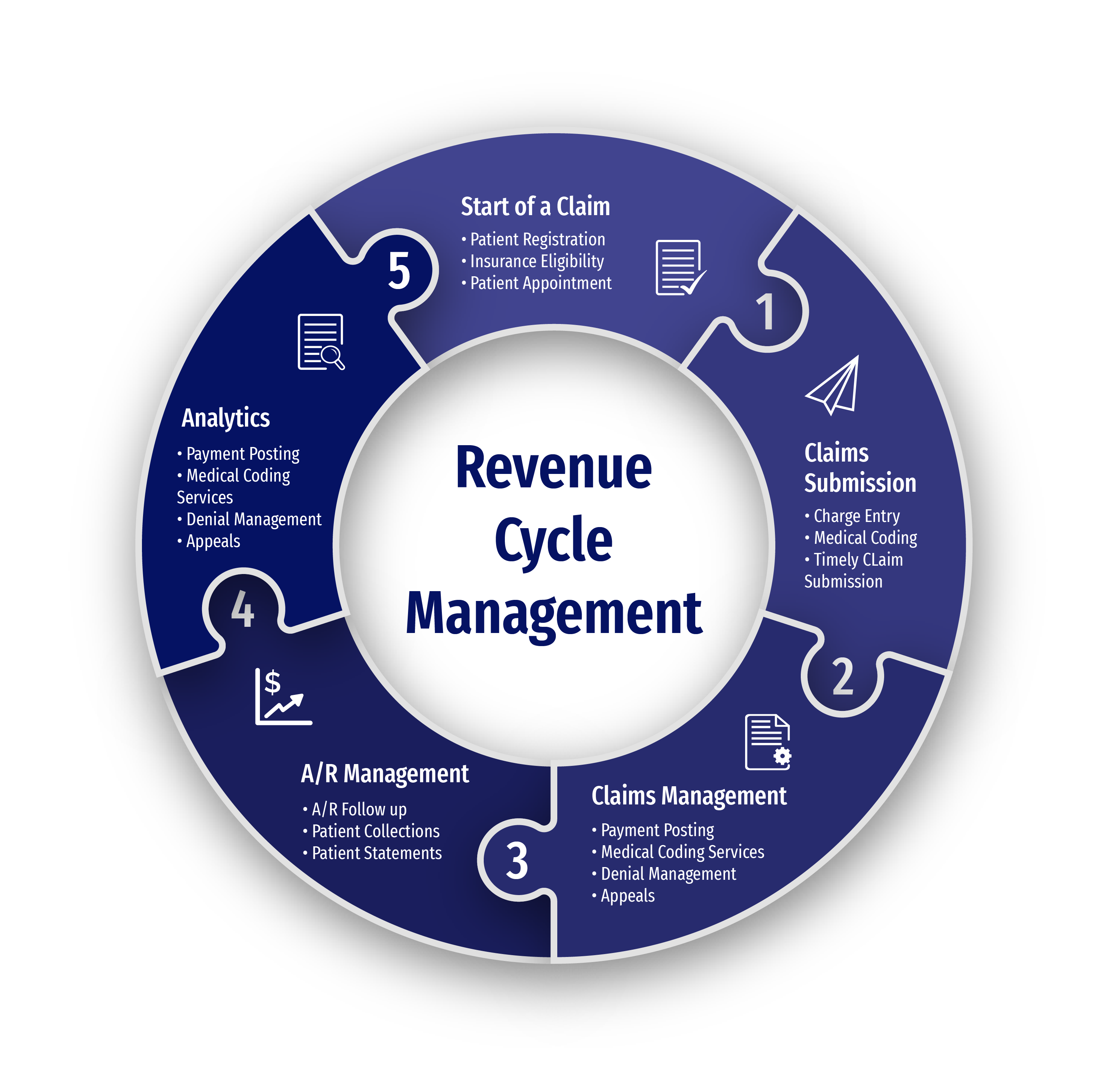
Our gastroenterology hepatology billing services are designed to improve workflow efficiency and ensure accurate financial processes. Below are the services we offer:
Accurate Coding for Liver Diseases
We ensure that all liver diseases, including cirrhosis, hepatitis, and liver cancer, are accurately coded to comply with billing and insurance guidelines.
Chronic Liver Disease Billing
Billing for chronic liver diseases such as Hepatitis B and Hepatitis C can be complicated. Our team ensures precise coding and the management of long-term treatment plans.
Diagnostic Procedures Coding
We handle the coding for diagnostic tests like liver biopsies and imaging, which are essential in diagnosing liver conditions.
Claims Submission and Denial Management
We streamline the claims process to ensure timely submissions and manage denials to prevent revenue loss.
Why Choose Us for Your Hepatology Billing?
Compliant Hepatology Medical Billing
We ensure all billing processes adhere to payer and state regulations, minimizing the risk of errors and penalties.
Maximized Reimbursements For Your Practice
Our accurate coding and billing practices lead to faster approvals and higher reimbursements for your hepatology practice.
Efficient Claim Management
We handle the full claim cycle, from submission to follow-up, ensuring timely payments and fewer delays.
Dedicated Hepatology Billing Team
Our team specializes in hepatology medical billing, ensuring accurate claims and reducing the risk of denials.

Challenges in Hepatology Medical Billing
Complex Coding Requirements
The variety of liver diseases, such as hepatitis, cirrhosis, and liver cancer, necessitates specific and accurate coding. Furthermore, procedures like biopsies, imaging, and liver transplants each require distinct codes, demanding a high level of expertise to ensure claims are correctly submitted.
Evolving Regulations
Hepatology billing must comply with ever-changing healthcare regulations and coding updates. Staying current with these changes is essential to avoid costly mistakes and ensure reimbursements are processed according to the latest guidelines for liver-related treatments.
Insurance Verification and Authorization Delays
Hepatology and gastroenterology treatments often require extensive insurance verification and prior authorizations, especially for high-cost procedures like liver transplants. Delays in obtaining approval can halt the billing process, affecting the overall revenue cycle and causing patient dissatisfaction.
Long-Term Chronic Disease Management
Billing for chronic liver conditions, such as Hepatitis C and cirrhosis, requires managing continuous care and treatment plans. The ongoing nature of these diseases, along with complex drug regimens and monitoring procedures, can complicate coding and reimbursement timelines.
Timely Claim Submissions
In hepatology and gastroenterology, timely claims are critical, as delays can result in disruptions to a practice’s cash flow. Claims for specialized treatments, such as biopsies or transplant-related services, require extra attention to detail to ensure they’re filed promptly to avoid delayed reimbursements.
Handling Denied Claims and Rejections
Denied claims are a common challenge in hepatology billing, often due to incorrect coding or missing information. Hepatology procedures can involve a high degree of complexity, making the appeal process time-consuming and requiring a deep understanding of both the medical and billing aspects to successfully resolve issues.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Hepatology billing involves a wide variety of liver diseases and treatments, each requiring specialized coding and documentation. Procedures like biopsies, imaging, and liver transplants demand a deep understanding of medical terminology and coding to ensure proper reimbursement and compliance.
Outsourcing your hepatology medical billing to an expert team ensures accurate coding, timely claims submission, and effective denial management. This leads to faster reimbursements, improved collections, and fewer billing errors, ultimately enhancing your practice's revenue cycle.
Yes, outsourcing to a professional hepatology billing company ensures your billing processes remain compliant with ever-evolving healthcare regulations. Our team stays up-to-date with the latest coding guidelines and payer requirements, so you don’t have to worry about costly compliance errors.
Our team at CLICKVISIONBPO handles the entire billing process, from accurate coding to timely claims submission. We prioritize efficient workflows to ensure your hepatology claims are submitted promptly, reducing delays and improving your revenue cycle.
