Effective revenue cycle management is essential for financial stability and operational efficiency in today’s healthcare environment. While the healthcare landscape constantly changes, navigating common complexities and intricacies can be challenging for many organizations. Optimizing financial outcomes requires a deep understanding of RCM processes. But do you know how to improve revenue cycle management?
Below, you’ll learn all about it!
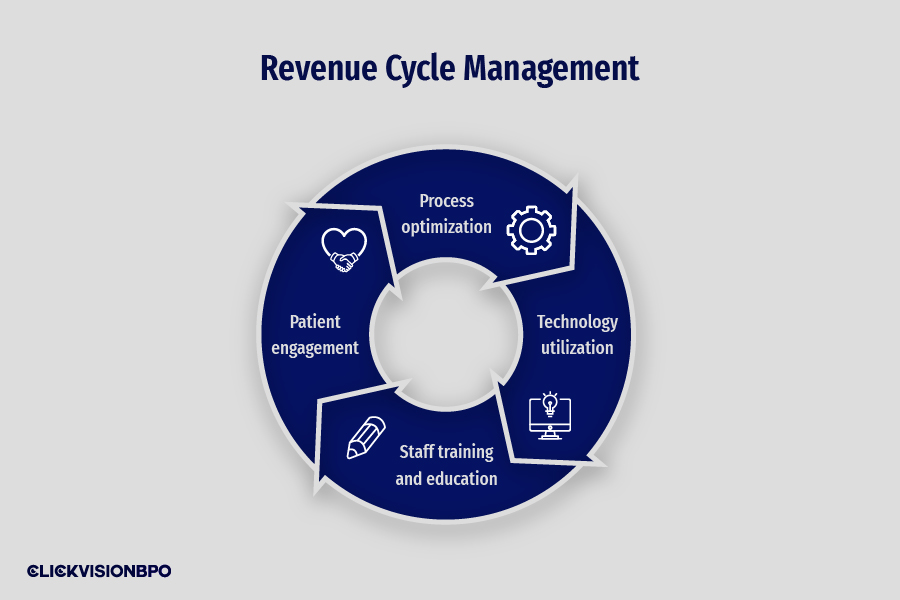
Revenue Cycle Management Strategies
Healthcare organizations constantly search for strategies to enhance and optimize their Revenue Cycle Management (RCM) processes to boost efficiency and financial health. By streamlining RCM, providers can alleviate common challenges faced by providers, including billing errors, delays in reimbursement, and increased administrative costs.
A well-optimized RCM process in place can significantly improve cash flow, reduce denials, and enhance the overall patient experience. This can all be achieved while maintaining a smooth billing process.
Below, we’ll discuss some of the best practices every healthcare organization should know on how to improve revenue cycle management for exceptional optimization. Here are the best ones:
Process optimization
Optimizing Revenue Cycle Management processes has become vital for any organization seeking success and sustainability. Achieving optimal RCM optimization goes beyond merely managing finances.
Its benefits extend to enhancing patient satisfaction and overall operational efficiency and speed within your clinic. While facing challenges in RCM is typical, they can be easily overcome by the following:
Streamlining patient registration and verification
Streamlining patient registration and verification is a crucial step for optimizing RCM, as it directly impacts revenue capture as well as subsequent billing and reimbursement processes. By automating the initial registration using EHR systems, you’ll save precious time, reduce errors, and ensure exceptional accuracy in data captured.
Additionally, implementing thorough insurance verification processes for patient eligibility and insurance coverage further streamlines workflow. This helps prevent errors and denials, ultimately supporting financial goals and enhancing patient experience.
Source: freepik.com / Photo Contributor: pressfoto
Enhancing coding accuracy
Coding accuracy is imperative for RCM. Accurate coding ensures that diagnoses and procedures are documented correctly, contributing to reduced claim denials and compliance with coding standards. By enhancing coding practices, your organization can enjoy improved revenue outcomes, enhanced operational efficiency, and save administrative burdens.
Deliver accurate and timely patient billing
Effective RCM strongly relies on accurate and timely patient billing practices. They are vital in improving patient experience and increasing revenue collection.
Providers can streamline financial processes by providing clear and comprehensive estimates, implementing effective billing and collection practices, and leveraging data-driven insights and automation. It may lead to significant increases in revenue and efficiency.
Improve payment collections processes
Improving payment collection processes can significantly optimize your organizational RCM, enhancing revenue capture and reducing bad debt. Offering patients multiple payment options increases the likelihood of capturing payments promptly and efficiently.
By incorporating patient payment portals, you can facilitate convenience and accessibility, allowing your patients to easily settle balances on their schedules. Thus, this approach will improve cash flow and ridicule billing-related challenges for your organization.
Technology utilization
Healthcare RCM processes generate vast amounts of data, demanding advanced technology for efficient management, analysis, and decision-making insights. By utilizing innovative solutions, providers can transform their operations and achieve streamlined workflow and improved financial outcomes. Some of the ways technology can optimize RCM include:
- Streamline workflow by implementing automated systems, online payment solutions, Electronic Health Records (EHR) integration, and RCM software solutions.
- Elevate staff productivity by utilizing RCM analytics and reporting tools for data-driven decision-making and streamlining operations with increased efficiency through system automation, reducing manual workloads.
- Ensure robust data security and compliance by adhering to HIPAA compliance measures, protecting sensitive data and encryption with secure mechanisms for storage and transmission, and identifying vulnerabilities while implementing continuous improvement measures with automated practices.
Staff training and education
Training and education of your staff is essential for effective operation due to the complex and comprehensive nature of RCM. From gathering patient data to collecting payments, each step in the revenue cycle is interconnected and crucial for operational performance and success.
With effective training, providers can ensure that members understand their roles and responsibilities, leading to enhanced accuracy, reduced errors, and maximized reimbursement. Training on the following key components equips staff with the necessary skills and knowledge to perform tasks effectively and accurately:
- Patient registration – Ensures accurate and efficient data collection during the initial registration, which is vital for claim processing.
- Insurance verification – Staff need to understand insurance verification processes to determine coverage, eligibility, and benefits, which will minimize reimbursement denials.
- Coding – Knowing medical coding practices and staying updated with coding changes is essential for assigning correct codes and optimizing reimbursement.
- Claim submission – Proper claim submission procedures reduce rejections and accelerate payment processing.
- Denial management – Enables staff to promptly investigate, appeal, and resolve claim denials, improving recovery and financial performance.
- Payment posting – Ensures accurate and timely application of payments to patient accounts.
- Compliance regulations – Knowing relevant compliance regulations like HIPAA ensures patient data privacy and adherence to legal requirements.
Patient engagement
Patient engagement is vital in revenue cycle management, positively impacting your healthcare organization’s financial performance. By optimizing patient experience, you can achieve several significant outcomes, from building long-term patient loyalty to enhancing practice profitability and efficiency. Some of the key strategies for involving patients in the financial aspects of their care include:
- Empowering patients with financial transparency for informed decision-making reduces billing disputes and enhances overall satisfaction.
- Facilitating convenient billing and payment options for a clear and proactive engagement in managing medical expenses.
- Enhancing patient communication and education to promote confidence and knowledge on insurance coverage, financial aid options, and billing processes.
- Promoting financial responsibility and accountability for empowering patients to make informed decisions improves financial health and reduces financial stress.
- Streamlining patient registration and insurance verification for accurate billing, reduced administrative errors, and improved revenue collection efficiency.
These measures collectively ensure quicker reimbursement and simplified claim processing. This leads to increased revenue capture through minimized billing errors and optimized payment processes while enhancing patient satisfaction.
Prioritizing patient engagement and financial transparency boasts profitability and efficiency and strengthens your relationship with patients. This fosters mutual trust and confidence.
How Can an Organization Improve Its Revenue Cycle Management?
To understand how to improve revenue cycle management, conducting regular RCM assessments to identify untapped opportunities helps you foster a culture of continuous improvement. By doing so, organizations can seamlessly adapt to evolving challenges and implement targeted solutions.
However, gaining valuable insight through performance metrics is essential for providers. They use such metrics to access measurable benchmarks to monitor performance, identify inefficiencies, and implement informed solutions and strategies for optimization.
These tools for tracking and monitoring are Key Performance Indicators (KPIs) that help evaluate organizational efficiency and areas for improvement and guide opportunities for optimizing RCM. Some of the key healthcare revenue cycle KPIs include:
- Days in accounts receivable (AR) – This represents the average days your company takes to collect payments after services are rendered.
- Clean claim rates – Measure the percentage of claims processed and paid by third-party insurers on initial submission without encountering any errors, delays, or inquiries.
- Denial rates – Measure the percentage of claims denied or rejected by third-party payers.
- Collections rates – Provide measurable benchmarks focusing on revenue collected for services rendered.
Revenue Cycle Management Outsourcing
Exploring the option of outsourcing certain aspects of RCM can offer significant advantages for healthcare organizations, from streamlining workflow to optimizing billing, coding, and collection practices. Partnering with an outsourcing agency like CLICKVISION BPO reduces costs compared to freelancers or maintaining in-house teams and leverages specialized experience and advanced technology.
Our capabilities expand beyond mere revenue cycle management practices, offering tailored solutions for maximizing revenue capture, supporting financial sustainability, and optimizing operational performance for healthcare facilities. By outsourcing critical tasks of RCM, you can focus on core functions within your clinic while benefiting from the efficiencies and expertise of our services.
Regulatory Compliance
Regulatory compliance refers to an organization’s efforts to ensure appropriate measures, and billing processes enable them to adhere to all legal and professional obligations. Since RCM in healthcare is subject to various legal and regulatory requirements, adherence to set guidelines is critical to avoid legal penalties, administrative burdens, fines, reputational damage, etc.
Maintaining compliance is a complex and demanding endeavor. You may manage the complexities and achieve operational excellence in RCM by being aware of the following rules that all healthcare firms are subject to the following:
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) sets robust standards and regulations for protecting sensitive patient data during revenue cycle management. Compliance with such requirements involves ensuring the security and confidentiality of health information by implementing appropriate mechanisms for safeguarding against unauthorized access or disclosure.
Medicare Access and CHIP Reauthorization Act
The Medicare Access and CHIP Reauthorization Act (MACRA) aims to transform healthcare payment systems toward value-based care by rewarding providers based on the quality of care provided over quantity. Compliance with MACRA regulations for RCM focuses on reporting quality measures, utilizing EHR technology, and actively improving activities mandated by the program.
Centers for Medicare and Medicaid Services
The Centers for Medicare and Medicaid Services (CMS) is responsible for administering Medicare, Medicaid, and other healthcare programs within the healthcare industry. Compliance with CMS in RCM involves adhering to specific guidelines to ensure accurate and appropriate billing, coding, documentation, reimbursement, and quality reporting.
Continuous Monitoring and Improvement
In the ever-evolving healthcare landscape, continuous monitoring and improvement in optimizing RCM processes are vital to adapt to changing regulations, trends, and advancements. To navigate these complexities and optimize financial outcomes, implementing proactive strategies enables providers to maintain sustainable financial performance and operational efficiency.
Thus, having a strong focus on data analytics, performance benchmarks, and regular assessments is imperative. It helps leverage data and drive informed decision-making on improvements and opportunities, minimize revenue leakage, and ensure compliance with regulatory requirements.

Source: freepik.com
Conclusion
Knowing how to improve revenue cycle management allows providers to optimize cash flow, reduce operational costs, and enhance overall financial performance. Reinforcing the importance of proactive approaches and ongoing evaluation of RCM ensures that your organization can identify and address errors and inefficiencies before they impact your revenue streams.
By maintaining continuous monitoring and improvement, you can achieve sustained financial success and maximize revenue collection while minimizing claim denials and adapting to changing regulatory and industry requirements. With CLICKVISION BPO’s innovative solutions, we guarantee streamlined revenue processing, driving operational efficiency and financial sustainability.
However, navigating these complex tasks can be challenging for many providers. So, CLICKVISION BPO offers tailored RCM solutions to enhance revenue capture and optimize operational efficiency for healthcare organizations. With a comprehensive understanding of common challenges, our team ensures accuracy in patient data input and coding practices and implements practical strategies to minimize denied claims.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
