Accurate insurance verification is a key component of revenue cycle management. It reduces administrative burdens, prevents claim denials, and improves patients’ financial transparency. Wondering how to verify insurance eligibility and benefits?
As professionals in outsourcing services in the healthcare and insurance industries, we are here to clarify your dilemma. We will equip you with the necessary knowledge of the verification process, which is crucial for a seamless and effective healthcare delivery.
About Accurate Insurance Verification
Imagine a scenario in which a patient receives treatment, assuming the insurance will cover it. They later discover that the claim is denied due to a lack of insurance coverage. This is absolutely not an ideal situation.
It can cause financial burdens for the patient as well as administrative challenges for the provider. For this reason, accurate insurance verification is crucial for various medical facilities such as clinics, hospitals, and nursing homes.
Insurance eligibility verification is a process that ensures that patients are eligible for the medical services they receive. It also helps healthcare providers avoid claim denials and costly reimbursement delays. Verification of benefits dives deeper and allows you to discover what exactly is covered by the payer for the patient.
Yet, the process entails more than confirming the patient’s insurance coverage. It requires an understanding of their coverage limits, doing a breakdown of benefits, as well as obtaining pre-authorizations.
Why is accurate insurance verification important?
Chasing misinformation and correcting errors can be a time-consuming and resource-intensive task. Proactive verification reduces the need for back-and-forth communication with insurance companies, streamlining the process.
Patient insurance verification entails confirmation of the validity of a patient’s insurance coverage details and identifying the benefits provided by the plan. This step ensures that the patient is eligible to receive specific medical services.
Since the patients understand their coverage beforehand, they can make educated decisions regarding their healthcare choices. On that note, the insurance providers can discuss potential costs upfront, which fosters trust and avoids financial surprises.
The importance of this process is evident in the fact that it ensures healthcare providers receive timely payments for the services they provide.

Source: freepik.com / Photo Contributor: user4894991
Pros of Accurate Insurance Eligibility and Verification for Healthcare Providers
When done correctly, the verification of insurance coverage can provide many advantages for medical providers. It enables medical providers to give quality care, knowing they will receive compensation for the services they provide.
The benefits also include:
- Minimization of denied claims – The verification of insurance coverage reduces the likelihood of claim rejections as a result of eligibility issues.
- Enhanced revenue cycle management – Due to the reduction of billing errors, the process accelerates claims processing and allows timely reimbursements.
- Reduction in administrative burdens – Efficient and accurate verification processes can alleviate administrative burdens for the staff and save them time for more critical tasks.
- Cash flow predictability – Knowing in advance that the patient’s services are covered by insurance leads to predictable cash flow.
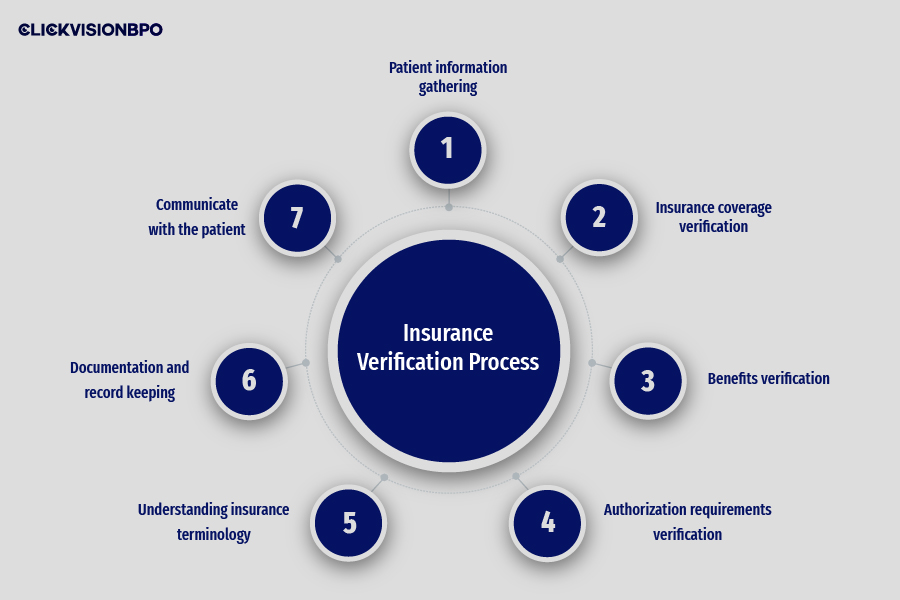
Insurance Verification Process
1. Patient information gathering
To verify the patient’s insurance coverage with ease, you have to obtain accurate and up-to-date information from the patient. The verification will help you identify their insurance plan, determine their payment responsibilities, and avoid any issues.
For a successful insurance verification, be sure to record:
- Patient demographics (name, date of birth, address) – These details help the insurance provider locate the correct patient record within their database.
- Insurance company name and contact details – By knowing the insurance company name and contact details, the provider can reach the right source of verification.
- Policyholder information (name and relationship to the patient) – This includes the name of the policyholder and their relationship to the patient.
- Policy number and group number – The unique policy number identifies the specific insurance plan within the company. The group number pinpoints the correct coverage details.
- Primary care physician information (if required) – Certain insurance plans require patients to see their primary care physician for a referral before they see a specialist. The PCP data allows the verification of this requirement.
2. Insurance coverage verification
After gathering the necessary patient information, the following step is to confirm the patient’s insurance coverage details. They will give you clear insights into the scope of medical services that the insurance plan covers.
You can perform a successful verification by calling the patient’s insurance provider and checking for the following:
- Checking the patient’s policy status (whether it is active or inactive) – This confirms whether the policy is in good standing. If it is inactive or canceled, it won’t provide coverage.
- Check the policy type – Determine what type of insurance the patient holds. Each type may have different requirements and limitations.
- Verifying the effective dates of the insurance coverage – It is crucial to ensure the insurance policy is active on the date of service to avoid any claim denials. The start and the end date of the coverage determine if the service falls within the valid coverage period.
- Identifying any network limitations (in-network or out-network providers) – Many insurance plans have in-network or out-network providers. You will need to verify if the provider is within the patient’s network for optimal benefits.
Most payers have online portals for verifying insurance coverage and it’s the most common way to verify a patient’s eligibility.
3. Benefits verification
This step involves a comprehensive understanding of the specific information available to the patient under their insurance plan. These details can help providers determine co-payments, co-insurance amounts, deductibles, out-of-pocket maximums, and any coverage limitations.
The benefits verification also ensures alignment between the provided services and the reimbursement benefits. Critical areas for exploration include:
- Coverage for office visits, procedures, diagnostic tests, and medications
- Specific details about the services that are covered (e.g., frequency limits)
4. Authorization requirements verification
Certain medical procedures require prior authorization from the insurance company. Accurate verification is crucial in this process, as failing to obtain necessary authorizations can lead to claim denials and delays in reimbursement.
Compliance with the authorization protocols can mitigate the risk of claim denials and reimbursement delays. The purpose of obtaining authorization is needed for:
- Confirming referrals to specialists
- Pre-certifications for specific medical procedures
5. Understanding insurance terminology
In order to accurately verify insurance eligibility and benefits, you need to be familiar with common insurance terminology. You must be able to interpret terms such as deductibles, co-payments, co-insurance, out-of-pocket maximums, etc.
Understanding such terms will help you accurately estimate patient financial responsibilities and navigate insurance claims effectively. Also, a clear grasp of the concepts facilitates accurate interpretation of benefits and financial obligations.
6. Documentation and record keeping
Throughout the verification process, you need to maintain detailed and accurate documentation. The insurance should document all interactions, such as verification results and authorization confirmations, with insurance companies.
Such record-keeping tasks facilitate transparency, compliance, and future references. It can also minimize errors and any discrepancies during the verification process and streamline future interactions with the insurers.
7. Communicate with the patient
Once you complete the verification process, inform the patient about their insurance eligibility status, their financial responsibilities, and other coverage details. Maintaining clear communication can help you manage the patient’s expectations and avoid any surprises or issues during the medical billing process.
Challenges in Insurance Verification
Now that we have explored how to verify insurance eligibility and benefits, let’s discuss some common challenges associated with this process.
Incomplete and accurate information
Receiving incomplete or inaccurate patient information is one of the most common challenges regarding insurance verification. Simple typos or outdated information can lead to errors like insurance claim denials as well as delays in reimbursement.
Complex insurance policies
Insurance policies vary in coverage, deductibles, copayments, and preauthorization requirements. The different types of services, plans, exclusions, deductibles, copays, and network variations can make deciphering the coverage challenging.
Understanding these nuances can be intricate, especially for staff members who are not well-versed in such terminology. Insurance coverage can change due to factors such as job transitions, life events, and other updates.
Hence, coverage verification must be performed in real time, as each insurance plan may have unique requirements. Keeping up with the plan updates can be a constant challenge for medical staff.
Limited access to information
Some insurance companies may have limited access to online verification portals. Others may require lengthy wait times when contacting a customer service representative. In fact, even with careful verification, the claims can be denied due to unforeseen coverage limitations, prolonging the insurance verification process.
Outsourcing insurance eligibility
Outsourcing the verification task can be very beneficial for healthcare providers. These third-party vendors have the necessary skills and tools to finish these tasks successfully, ensuring they are handled accurately and effectively.
Strategies for Overcoming Insurance Verification Challenges
As you can see, insurance eligibility and insurance verification can be a challenging task. Luckily, at CLICKVISION BPO, we have a deep understanding of the need for outsourcing services and unique solutions in this sector.
We provide customized solutions based on the business’s needs and requirements. In continuation, we will provide you with some strategies that can help you overcome hardships during the verification process.
Establish standardized procedures
One way to simplify the process and avoid claim denials is to implement standardized procedures for collecting patient information. You can create checklists or templates to ensure the staff members gather the necessary data consistently.
Take advantage of technology
Investing in software solutions can help you streamline the whole process. Tools like electronic verification systems or billing software with built-in eligibility checks can automate data entry, improve accuracy, and reduce manual errors. Such systems connect directly with insurance companies for faster and more accurate results.
Maintain clear communication channels
To achieve a successful verification process, we recommend you maintain open lines of communication with the insurance companies. Doing so also enables you to address any challenges promptly and efficiently. You can also encourage patients to review and update their insurance information on a regular basis to minimize errors.
Monitor key performance indicators (KPIs)
Monitoring key performance indicators can also be very beneficial during the verification process. Whether it is verification turnaround time, claim denial rates, or reimbursement accuracy, data analysis can help you track areas of improvement and implement suitable strategies accordingly.
Training and Education
Providing suitable ongoing training and education is essential when it comes to insurance verification. This includes offering workshops, seminars, and online courses to enhance staff’s knowledge of insurance policies and practices.
You can cross-train staff members across different departments to ensure they are proficient in performing verification tasks. Doing so ensures continuity in operations and helps mitigate the risk of staff turnover.
Understanding the best practices and proper data collection minimizes the risk of errors. Moreover, an extensive knowledge of the insurance plans and procedures can save time and resources.
You can also hire a business solution company, such as CLICKVISION BPO, offering services designed to meet the diverse needs of healthcare organizations. Our team has expertise in medical billing processes and will ensure a seamless process.

Source: freepik.com / Photo Contributor: pressfoto
Conclusion
In this guide, we explored how to verify insurance eligibility and benefits effectively. This process is crucial for ensuring billing and facilitating timely reimbursements. In fact, by navigating each verification step, healthcare providers can enhance operational efficiency and prevent administrative burdens. It enables them to deliver top-quality care while managing the financial aspect of patient treatment effectively.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
