- Home
- »
- Specialties
- »
- Neurology Billing Services
Neurology Billing Services | Neurology Billing Company
Neurology is a medical specialty focused on diagnosing and treating disorders of the nervous system, which includes the brain, spinal cord, nerves, and muscles. From common conditions like headaches and epilepsy to more complex diseases such as multiple sclerosis and Parkinson’s, neurology encompasses a broad spectrum of care. Given the complexity and variety of neurological services, accurate and efficient billing is essential for proper reimbursement and regulatory compliance.
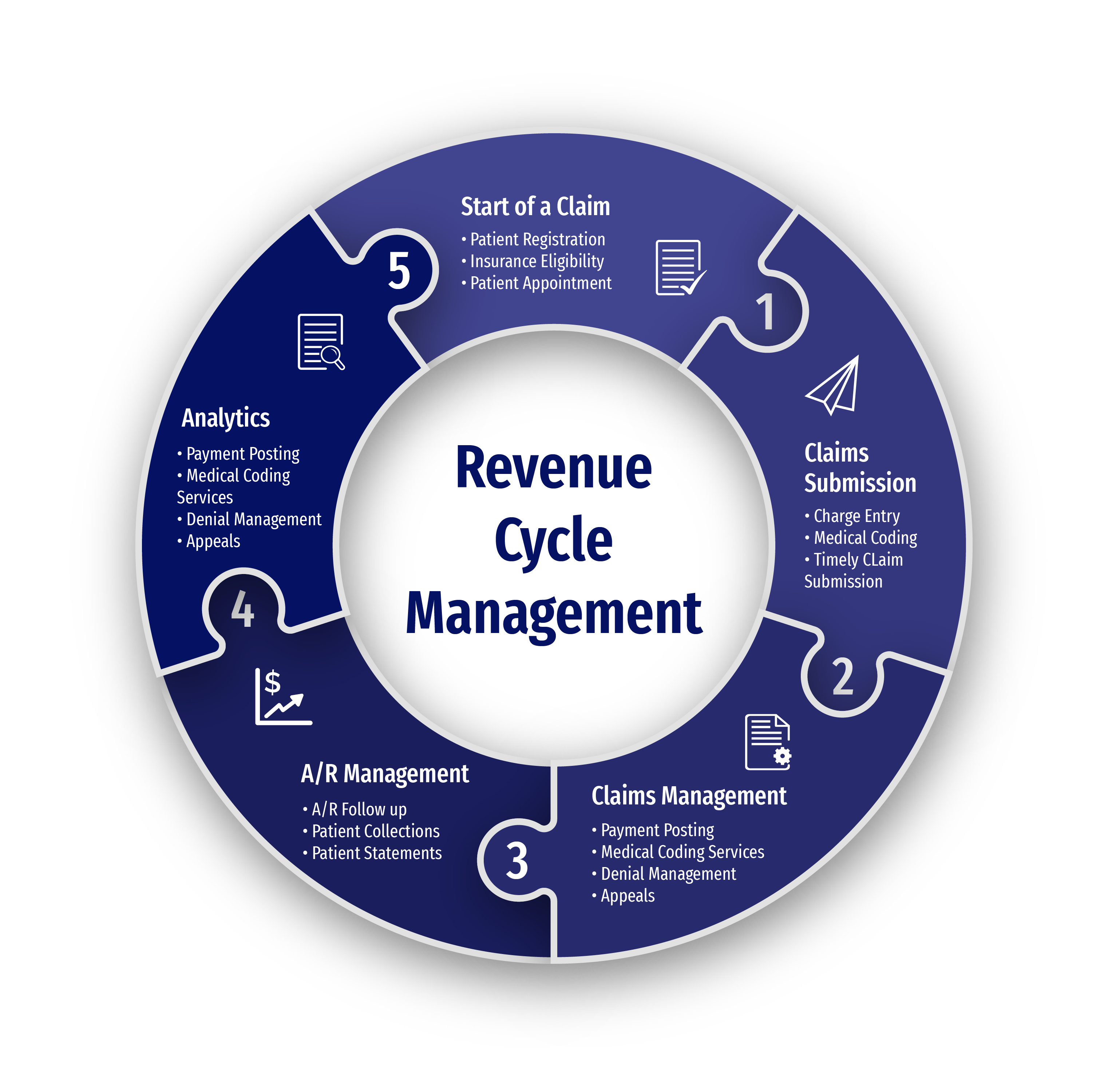
Our neurology billing services ensure that all aspects of your practice’s billing process are streamlined and optimized for maximum efficiency. As a trusted neurology medical billing company, we provide tailored solutions that manage everything from complex coding to timely claim submission, so you can focus on patient care and enhance your practice’s revenue cycle.
Comprehensive Neurology Billing Solutions
Our billing services are designed to meet the unique needs of neurology practices. We offer comprehensive solutions to ensure every aspect of your billing process is optimized for maximum efficiency and reimbursement.
Diagnostic Procedure Billing
Neurology practices often rely on complex diagnostic tests, such as EEGs, EMGs, and MRIs. We ensure these procedures are accurately coded, minimizing claim rejections and delays by adhering to payer-specific guidelines.
Chronic Condition Management Billing
Managing chronic neurological conditions, such as epilepsy, Parkinson’s disease, or multiple sclerosis, requires ongoing care. We track and document these services, ensuring timely and accurate reimbursement for long-term treatments.
Neurological Surgery Billing
For surgeries such as spinal procedures or brain surgeries, accurate coding is essential. We handle these intricate billing processes, ensuring all services are correctly documented and reimbursed without delay.
Pre-Auths for Specialized Procedures
Certain advanced treatments, including spinal cord stimulation or deep brain stimulation, require pre-authorization. We handle this process efficiently, securing approvals promptly and preventing delays in patient care.
Billing for Emergency Neurological Care
Emergent neurological services, like acute stroke care or trauma, require quick and precise claim submissions. We ensure no delays in the billing process, optimizing your practice’s revenue.
In-Hospital and Neurocritical Care Billing
For neurologists providing in-hospital care, including neurocritical care, the billing process can be intricate. Our team ensures accurate documentation and billing for these services, preventing errors and delays in reimbursement.
Benefits of Outsourcing Neurology Billing Services With Us
Compliant Neurology Medical Billing
We ensure that all billing processes for neurology services strictly comply with payer and state regulations, reducing errors and avoiding costly penalties. Our commitment to compliance safeguards your practice from financial setbacks.
Maximized Reimbursements for Your Practice
Through accurate coding and meticulous attention to detail, we help your practice achieve quicker claim approvals and increased reimbursements. Our expertise ensures you receive the financial outcomes you deserve.
Efficient Claim Management
From claim submission to follow-up, we manage the entire claim cycle, ensuring timely payments and minimizing delays. Our proactive approach keeps your practice’s cash flow steady and reduces revenue disruptions.
Dedicated Neurology Billing Team
Our team of specialists is focused on neurology billing, providing in-depth knowledge of the unique billing needs for each neurology service. This reduces the risk of claim denials and ensures your practice’s billing is handled with expertise.

Challenges of Neurology Billing and Solutions
Complexity of Neurology Procedures
Neurology involves a wide range of complex procedures like EEGs, EMGs, and nerve conduction studies, which require precise coding. Errors in documentation or coding can lead to claim denials. We ensure accurate coding for all services, reducing the risk of denials and optimizing reimbursements.
Pre-Auths Requirements for Specialized Treatments
Treatments like deep brain stimulation or advanced imaging often require pre-authorization, which can delay the approval process. Our team handles pre-authorization efficiently, securing approvals to avoid interruptions in patient care and billing.
Billing for Chronic Neurological Conditions
Conditions such as epilepsy, Parkinson’s, or multiple sclerosis require ongoing care and billing for multiple services over time. We track all treatments, ensuring proper documentation and coding for consistent and timely reimbursements.
Frequent Insurance Variations
Insurance companies may have different policies for neurology procedures, leading to discrepancies in coverage. We stay updated on payer-specific requirements and ensure that claims are submitted accurately to minimize delays and denials.
High Volume of Claims and Claims Follow-ups
Neurology practices often deal with a high volume of claims, making it easy for some to slip through the cracks. Our team actively follows up on all claims, ensuring timely payments and addressing any issues that may arise quickly.
Billing for Telemedicine Services
Telemedicine has become increasingly common in neurology, especially for consultations and follow-ups. We ensure that telemedicine services are billed appropriately, adhering to both payer guidelines and compliance standards to prevent issues with reimbursement.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Specialties We Excel In
Psychiatry Billing Services
Neurology and psychiatry often intersect when addressing mental health conditions with neurological roots, such as epilepsy or neurodegenerative diseases. Psychiatrists provide care for mental health, while neurologists focus on neurological aspects, collaborating to offer comprehensive treatment.
Behavioral Health Billing Services
Neurologists and behavioral health professionals work together to manage conditions like cognitive disorders, dementia, and mood disorders. Neurology focuses on the brain’s physical health, while behavioral health services address the psychological and emotional aspects, providing holistic patient care.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Outsourcing medical billing to CLICKVISION can lead to significant financial and operational benefits. Our expertise in neurology billing ensures accurate and timely claim submissions, reducing claim denials and optimizing revenue. This allows your practice to focus on patient care while improving cash flow and reducing overhead costs.
At CLICKVISIONBPO, we have a dedicated quality control team that double-checks all billing processes before submission. This team ensures that all claims comply with coding guidelines and payer requirements, minimizing errors and reducing the risk of claim denials and audits.
Compliance is a top priority at CLICKVISIONBPO. We adhere to all relevant industry regulations and stay updated with the latest billing guidelines in our outsourcing neurology billing solutions. Our team ensures that all neurology billing practices meet necessary compliance standards, safeguarding your practice from potential legal and financial risks.
Yes, we offer customized rheumatology billing solutions tailored to meet the specific requirements of your practice. Our personalized approach ensures that you receive the most effective and efficient billing solutions, addressing your unique challenges and optimizing your revenue cycle.
