Revenue Cycle Management Services for Ohio Providers
For healthcare providers in Ohio, the increasing complexity of payer requirements, frequent updates to billing codes, and pressure to maintain financial performance have made revenue cycle management (RCM) a critical priority. That’s why many medical practices, hospitals, and specialty clinics across Ohio are choosing to outsource revenue cycle management services to streamline operations and improve cash flow.
By partnering with us for RCM services in Ohio, healthcare providers can focus more on delivering quality patient care while we handle the administrative burden. Our comprehensive solutions include everything from insurance eligibility verification and charge capture to denial management and accounts receivable follow-up — all tailored to meet the unique regulatory and operational needs of Ohio-based practices.
Key Revenue Cycle Management Services for Ohio Providers
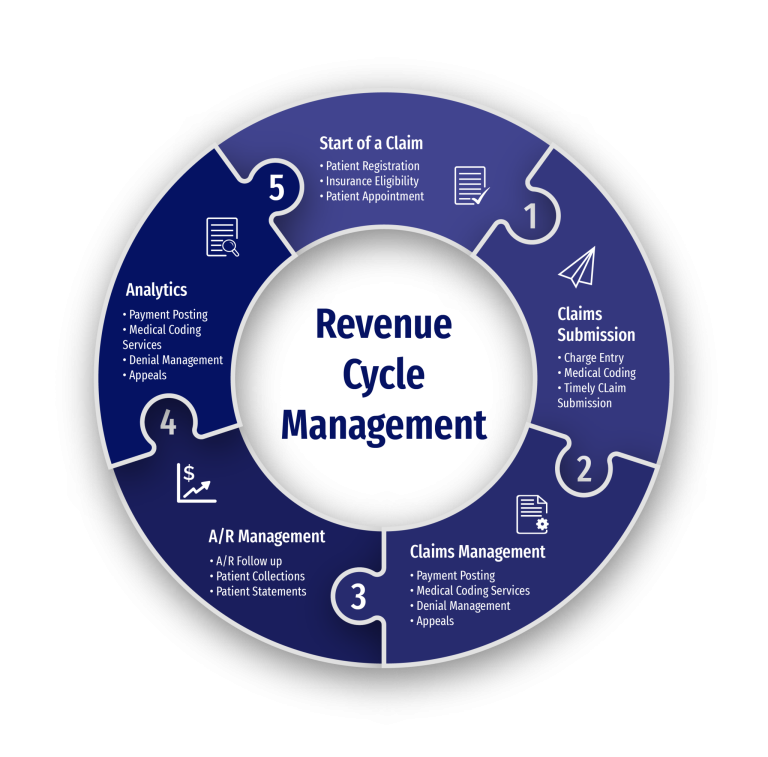
We offer full-spectrum revenue cycle management services designed to help Ohio healthcare providers improve efficiency, reduce claim denials, and accelerate reimbursements. Our outsourced RCM solutions support every phase of the revenue cycle, ensuring accurate data, timely billing, and consistent follow-up.
Insurance Eligibility & Verification
We verify patient insurance coverage and benefits before services are rendered, helping prevent costly denials and ensuring smoother claim processing.
Charge Capture & Coding Accuracy
Our team ensures that all services are accurately captured and coded according to current CPT, ICD-10, and HCPCS standards. This minimizes errors and supports faster claim approval.
Claims Submission & Tracking
We handle electronic and paper claim submissions to insurance carriers, ensuring compliance with Ohio-specific payer rules and reducing turnaround times.
Denial Management & Appeals
When claims are denied, we proactively manage appeals and rebilling to recover revenue efficiently. Our experts identify patterns and implement fixes to reduce future denials.
Payment Posting & Reconciliation
Our team records all incoming payments, matches them with claims, flags discrepancies, and provides clear financial reporting for your internal tracking.
Accounts Receivable (A/R) Follow-Up
We monitor aging accounts and follow up on unpaid or underpaid claims, working to reduce days in A/R and improve overall cash flow for your practice.
Revenue Cycle Challenges Ohio Healthcare Providers Face
Healthcare providers across Ohio face growing pressure to manage financial performance while navigating evolving payer rules, complex coding systems, and rising operational costs. These common challenges highlight the need for effective and efficient revenue cycle management services:
Evolving Payer Requirements
Ohio providers must constantly adapt to changes in insurance policies, reimbursement models, and payer-specific guidelines, making RCM more complex and time-consuming.
High Volume of Claim Denials
Denied claims remain a leading cause of revenue loss. Without dedicated denial management, practices risk delays in payment and unnecessary write-offs.
Operational & Staffing Costs
Maintaining an in-house billing and RCM team can be costly. Hiring, training, and managing staff — plus investing in RCM technology — places a heavy financial burden on many Ohio practices.
Lack of Visibility in Financial Performance
Many providers lack the tools or bandwidth to track revenue KPIs, monitor claims in real time, or make informed financial decisions based on data.
How Our Revenue Cycle Management Services Support Ohio Providers
Our tailored revenue cycle management solutions help healthcare providers across Ohio navigate billing complexities, reduce administrative burden, and optimize financial performance. By outsourcing revenue cycle management to our experienced team, your practice can streamline operations and improve profitability — without sacrificing patient care.
End-to-End Workflow Optimization
We manage the entire revenue cycle — from patient registration to final reimbursement — using best practices and technology to reduce delays and maximize collections.
Reduce Administrative Costs
By outsourcing RCM, Ohio providers eliminate the need for in-house billing staff, costly software investments, and ongoing compliance training — all while maintaining high performance and accuracy.
Improved Cash Flow & Faster Payments
Our proactive claims management, denial resolution, and A/R follow-up ensure quicker reimbursements and fewer outstanding balances on your books.
Scalable Solutions for Any Practice Size
Whether you’re a solo practitioner or part of a multi-specialty network, our RCM services for Ohio providers scale with your needs — offering flexibility and efficiency at every stage of growth.
Industries We Serve with Revenue Cycle Management in Ohio
Our revenue cycle management services are designed to support a wide range of healthcare providers across Ohio. Whether you're a small practice or a large healthcare facility, we bring specialized RCM expertise to help you increase collections and focus more on patient care.
-
Physician Practices
From general practitioners to specialists, we help Ohio physicians optimize claim submissions, reduce denials, and streamline their revenue cycle. -
Dental Offices
We manage dental RCM workflows — including CDT coding, insurance billing, and patient collections — ensuring timely reimbursements and fewer administrative tasks. -
Urgent Care Centers
For fast-paced care environments, our RCM services support accurate billing and real-time claim tracking, minimizing revenue leakage. -
Hospitals & Medical Centers
We work with hospitals and multi-location networks to handle complex billing processes, payer mix analysis, and comprehensive revenue cycle reporting. -
Ambulatory Surgery Centers (ASCs)
Our RCM solutions are tailored to ASCs in Ohio, offering precise coding, efficient charge capture, and accelerated payment cycles. -
Behavioral Health Providers
We assist behavioral health professionals and substance abuse clinics with specialized RCM services that address unique coding, documentation, and billing challenges.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Serving All Ohio
Help center
Got a question?
Get your answer!
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Outsourcing RCM allows Ohio providers to reduce administrative workload, improve cash flow, minimize claim denials, and ensure compliance with local and federal billing regulations. It also eliminates the overhead of managing in-house billing teams and software.
We use a proactive approach that includes accurate charge capture, timely claims submission, denial resolution, and consistent follow-up on accounts receivable. This results in faster payments and fewer write-offs for Ohio providers.
Absolutely. Whether you're a solo provider or a growing multi-location group, our RCM solutions are fully scalable and flexible to accommodate evolving needs, new specialties, or additional services.
Yes. Our RCM team is experienced with major insurance providers operating in Ohio and stays up to date with state-specific payer rules, Medicaid requirements, and commercial carrier policies.
