- Home
- »
- Specialties
- »
- Ophthalmology Billing Services
Ophthalmology Billing Services | Ophthalmology Billing Company
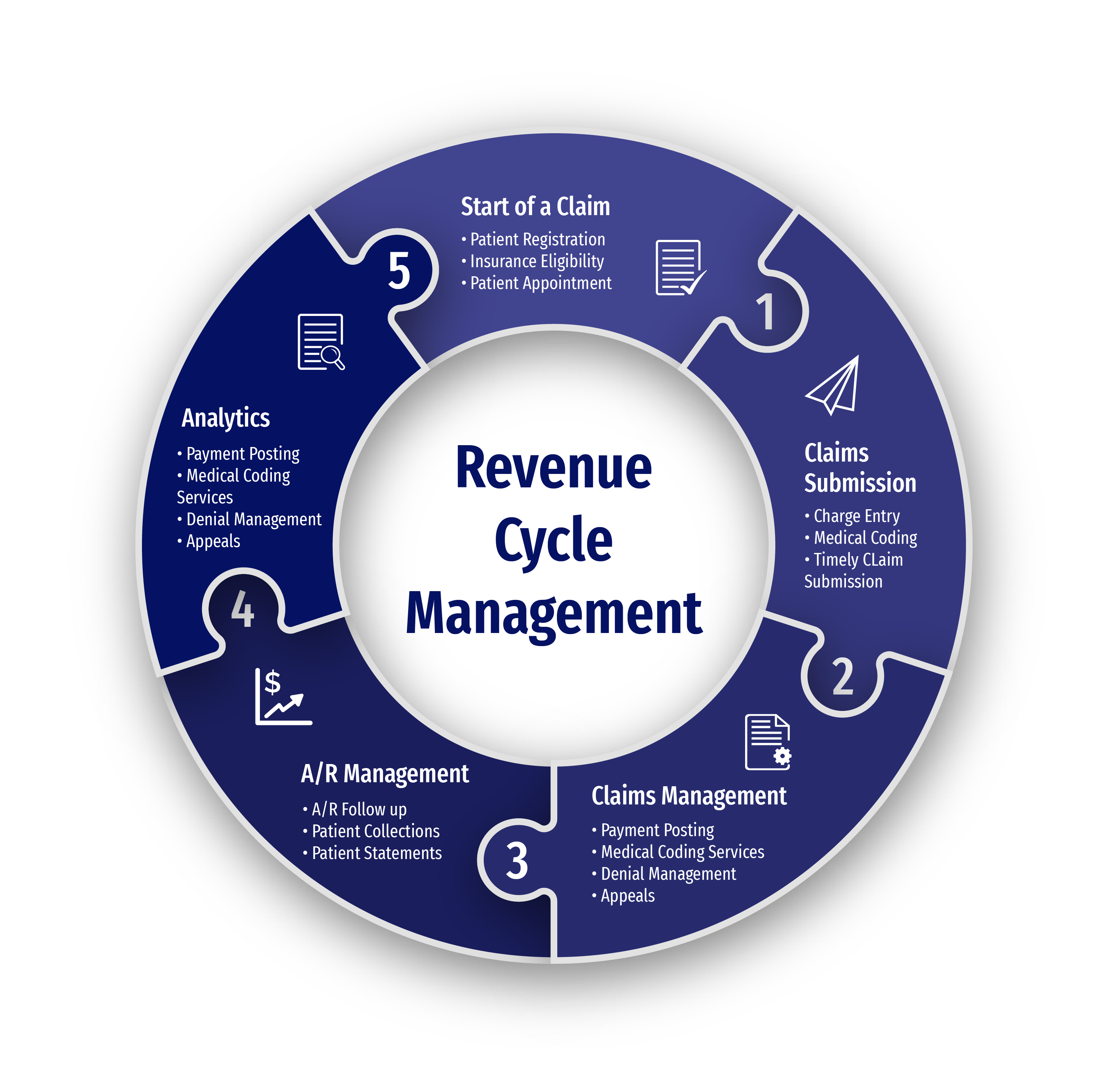
At CLICKVISIONBPO, we understand the unique challenges that come with ophthalmology billing services. As a top ophthalmology billing company, we manage complex coding requirements and ensure compliance with ever-evolving regulations, offering comprehensive billing solutions to streamline your revenue cycle management.
Our dedicated team of experts knows the ins and outs of ophthalmology billing, ensuring that every claim is processed accurately and timely, minimizing denials, and optimizing your revenue. By partnering with us, you can focus on delivering exceptional patient care while we handle the intricacies of ophthalmology revenue cycle management.
Comprehensive Ophthalmology Billing Solutions
Our ophthalmology billing services are tailored to meet the specific needs of eye care providers. Whether you manage a private clinic, a group practice, or a hospital, we have the expertise to handle your billing needs effectively.
Cataract and LASIK Surgery Billing
Surgical procedures like cataract removal or LASIK often involve complex coding and pre-authorization. We ensure all codes are accurately applied and required authorizations obtained to maximize reimbursements.
Billing for Glaucoma and Retinal Treatments
Managing chronic conditions such as glaucoma or macular degeneration requires precision. We handle the nuances of these cases to ensure accurate documentation and timely claim submission.
Routine and Preventative Eye Care Billing
From vision tests to preventative screenings, our team ensures seamless billing for routine services. We handle claims for both medical and vision plans, reducing delays.
Revenue Analytics and Performance Tracking
Our billing solutions include advanced analytics to provide insights into your revenue cycle. Track your financial performance and identify areas for improvement effortlessly.
Why Partner With Us For Ophthalmology Billing?
Partnering with us provides more than just billing services—it offers peace of mind. Here’s what sets us apart:
Expertise in Vision and Medical Plans
We understand the complexities of managing claims under vision and medical plans, ensuring every service is billed to the correct payer.
Seamless System Integration
We ensure our billing solutions align perfectly with your EHR and practice management systems, enabling efficient workflows and error-free data management.
Specialized Knowledge in Ophthalmology Procedures
Our team is trained in ophthalmology-specific billing codes and compliance requirements, guaranteeing accurate claim submissions.
Faster Payments and Lower Denials
Through meticulous claim preparation and proactive follow-ups, we reduce denials and speed up reimbursements, improving your cash flow.

Challenges in Ophthalmology Billing and How We Solve Them
Differentiating Vision vs. Medical Claims
Ophthalmology practices often provide services that fall under both vision and medical insurance, such as routine eye exams and treatments for glaucoma or cataracts. Incorrectly identifying the appropriate payer can lead to claim denials or delays. Our team carefully reviews each service and routes claims to the correct insurance provider, ensuring accurate and efficient reimbursements.
Managing Surgical Procedure Complexity
Procedures like cataract extraction, retinal detachment repair, or LASIK surgery involve intricate coding and thorough documentation. Missing details or errors in the coding process can lead to denied claims or underpayments. Our billing specialists are well-versed in ophthalmology-specific procedures, ensuring every surgical claim is detailed, accurate, and compliant with payer requirements.
Insurance Coverage Gaps in Routine Care
Routine eye exams and screenings are often excluded from medical insurance, leading to confusion and disputes over coverage. Misunderstanding these exclusions can result in denied claims or lost revenue. We work to identify coverage gaps, verify insurance benefits in advance, and guide practices in recovering reimbursements for eligible services.
Frequent Regulatory Updates
Ophthalmology billing codes, modifiers, and payer guidelines change frequently, and failing to stay compliant can disrupt the revenue cycle. Our team continuously monitors industry updates and applies them to your billing processes, ensuring every claim meets the latest standards. This proactive approach minimizes errors and keeps your practice financially secure.
Handling High Patient Volume
Busy ophthalmology practices often face backlogs in billing, particularly during peak seasons or promotional campaigns for elective procedures. Delayed submissions can strain cash flow and disrupt operations. By implementing efficient workflows and leveraging advanced billing technologies, we ensure that all patient services are billed promptly, accurately, and with minimal administrative burden.
Addressing Reimbursement Delays
Insurance companies often delay reimbursements for ophthalmology services due to incomplete documentation or verification errors. These delays can negatively impact cash flow and operational efficiency. Our billing experts proactively track claim statuses, address payer requests, and resolve issues to expedite payments, ensuring your revenue cycle runs smoothly.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Related Specialties We Excel In
Optometry Billing Services
Ophthalmology and optometry both focus on eye care, with ophthalmology specializing in medical and surgical treatment while optometry focuses on vision correction and routine eye exams. Our Optometry Billing Services handle claims for eye exams, prescriptions, and vision therapies, complementing ophthalmology treatments for comprehensive patient eye care.
Anesthesia Billing Services
Anesthesia plays a crucial role in ophthalmic surgeries, such as cataract removal or corrective eye procedures. Our Anesthesia Billing Services ensure accurate billing for anesthesia administration during these surgeries, allowing ophthalmologists to focus on patient care while we handle the complexities of anesthesia claims.
Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Our medical billing services streamline the entire billing process, from charge capture to claim submission and follow-up. By ensuring accurate coding and timely claim submissions, we minimize denials and optimize reimbursement rates, thereby improving your overall revenue cycle management.
At CLICKVISIONBPO, we prioritize compliance with all healthcare regulations, including HIPAA. Our team regularly updates their knowledge on the latest billing guidelines and payer requirements, ensuring that all claims are processed in compliance with industry standards. We also conduct regular audits to maintain high compliance standards.
Yes, we offer customized billing solutions tailored to the unique requirements of each ophthalmology practice. Whether you need full-service billing or specific support in certain areas, we work closely with you to develop a personalized plan that meets your specific needs and goals.
Yes, we offer customized rheumatology billing solutions tailored to meet the specific requirements of your practice. Our personalized approach ensures that you receive the most effective and efficient billing solutions, addressing your unique challenges and optimizing your revenue cycle.
Choosing the right ophthalmology billing company is crucial for optimizing your revenue cycle. At CLICKVISIONBPO, we stand out among ophthalmology billing companies by offering tailored solutions that reduce claim denials, ensure compliance, and improve cash flow. Our expert team is dedicated to providing accurate and timely billing services, allowing you to focus on delivering exceptional patient care while we manage your revenue cycle efficiently.
