- Home
- »
- Specialties
- »
- Psychiatry Billing Services
Psychiatry Billing Services
At CLICKVISIONBPO, we recognize the complexities involved in billing for psychiatric services. Our psychiatry billing services are designed to address the unique challenges faced by psychiatric practices, ensuring accurate billing, compliance with industry standards, and optimized revenue cycles.
With our comprehensive solutions, we help psychiatric providers focus on delivering exceptional care to their patients while we manage their billing needs efficiently.
Key Services
We are here to provide psychiatry billing services, ensuring a smooth operational workflow. Here's what we can assist with:
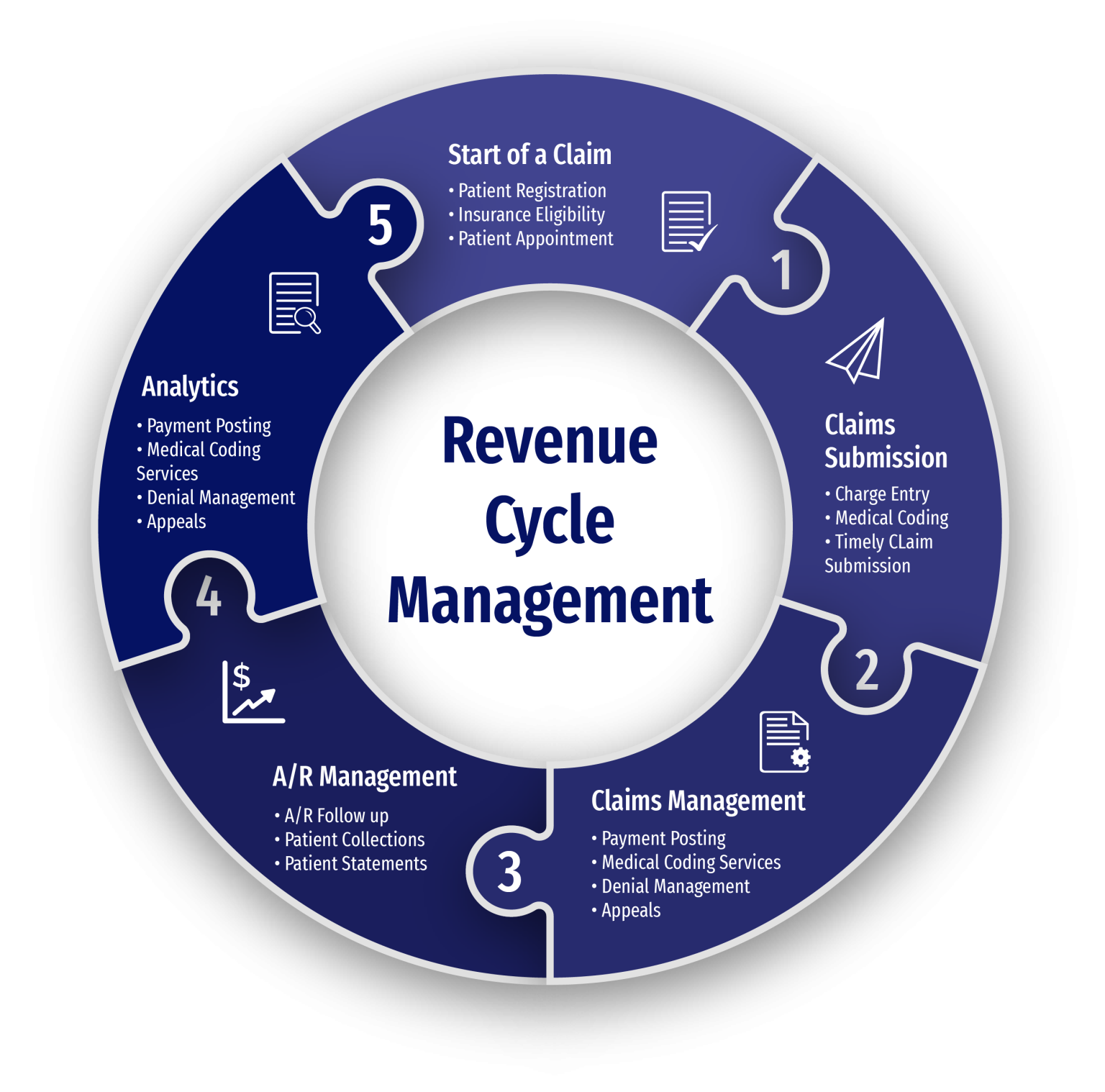
Psychiatry Revenue Cycle Management Services
-
Appointment Scheduling
-
Patient Registration
-
Insurance Verification
-
Charge Entry
-
Claim Status and Follow-up
-
Payment Posting
-
AR Management
-
Rejections
-
Denial Management
Benefits of Outsourcing with Us
Cost Effective Support
Access remote healthcare back office support at competitive rates, ensuring increased cost-savings.
Operational Efficiency
Optimize your budget with streamlined processes and reduced overhead costs, allowing for efficient resource allocation.
Scalability Option
Quickly upscale healthcare operations without the burden of hiring and training additional staff.
Dedicated Team
Count on a team assigned to your healthcare organization, providing tailored support according your operational policies.

Why Use Our Psychiatry Billing Services?
Specialized Expertise
Our team consists of highly skilled professionals who specialize in psychiatry medical billing services. They possess a deep understanding of psychiatric billing codes, insurance requirements, and regulatory standards. This expertise ensures that all billing activities are handled with precision and accuracy, reducing the risk of errors and claim denials. Our specialists stay updated with the latest changes in the mental health billing landscape, providing you with reliable and knowledgeable support.
Improved Cash Flow
With our optimized processes and streamlined workflows, we ensure prompt and accurate claim submission. Our team meticulously reviews documentation to ensure compliance with coding guidelines and payer requirements, minimizing claim denials and optimizing revenue. This results in faster reimbursements and improved cash flow, allowing your practice to maintain financial stability and growth. By partnering with us, you can focus on patient care while we manage your billing processes efficiently.
Efficiency and Accuracy
Our commitment to efficiency and accuracy sets us apart. We utilize cutting-edge billing software and implement best practices to ensure that all claims are submitted promptly and correctly. Our proactive approach includes regular audits and quality checks to identify and rectify any potential issues before they impact your revenue cycle. This dedication to accuracy minimizes delays and maximizes your practice's revenue potential.
Cost-Effective Solutions
Outsourcing your billing to CLICKVISIONBPO offers significant cost savings compared to managing billing in-house. You can avoid the overhead costs of hiring and training billing staff, as well as investing in billing software and infrastructure. Our transparent pricing models and flexible service packages ensure that you receive maximum value for your investment in our Psychiatry Billing Services. We help you reduce operational costs while maintaining high standards of billing accuracy and efficiency.
Tailored Solutions
We understand that every psychiatric practice has unique needs. That's why we offer tailored psychiatry billing services to meet your specific requirements. Whether you need assistance with insurance verification, claim submission, denial management, or patient billing, we customize our services to suit your practice's needs. This personalized approach ensures that you receive the support you need to achieve your financial goals.
Focus on Patient Care
By outsourcing your billing to us, you can free up time and resources to focus on providing quality care to your patients. Our comprehensive Psychiatry Billing Services handle all aspects of the billing process, from charge capture to denial management. This allows you to dedicate more time to patient care and practice growth, knowing that your billing operations are in capable hands.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Related Specialties We Excel In
Behavioral Health Billing Services
Psychiatry and behavioral health services often go hand in hand, especially when treating mental health disorders. Our Behavioral Health Billing Services support practices that focus on counseling, therapy, and other non-medication-based treatments, complementing psychiatric care and addressing the full spectrum of mental health needs.
Neurology Billing Services
Psychiatry and neurology frequently intersect, especially when dealing with conditions that affect both mental and neurological health. Our Neurology Billing Services simplify billing for diagnostic procedures, treatments, and neurological consultations, which often overlap with psychiatric care in cases involving cognitive disorders, depression, and other neurological conditions.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Outsourcing your billing to CLICKVISIONBPO can significantly benefit your practice by improving cash flow, reducing operational costs, and ensuring accurate and timely claim submissions. Our expertise in psychiatric billing allows you to focus on patient care while we manage your revenue cycle efficiently.
Our denial management process involves thoroughly analyzing denied claims, identifying the root causes, and promptly rectifying any issues. We resubmit corrected claims to ensure that you receive the reimbursement you deserve, minimizing revenue loss.
Absolutely. We understand that every psychiatric practice is unique, and we offer customized psychiatry billing services tailored to your specific needs. Whether you require assistance with insurance verification, claim submission, or patient billing, we can tailor our services to meet your requirements.
Our transition process is designed to be seamless and efficient. We conduct a thorough assessment of your current billing operations, develop a customized transition plan, and provide comprehensive training and support to ensure a smooth handover. Our goal is to minimize disruption and ensure continuity of service.
