- Home
- »
- Specialties
- »
- Behavioral Health Billing Services
Behavioral Health Medical Billing Services
At CLICKVISIONBPO, we recognize the unique complexities associated with billing for behavioral health services. Our behavioral health billing services are designed to navigate the specific challenges of this field, ensuring that mental health providers receive accurate and timely reimbursements.
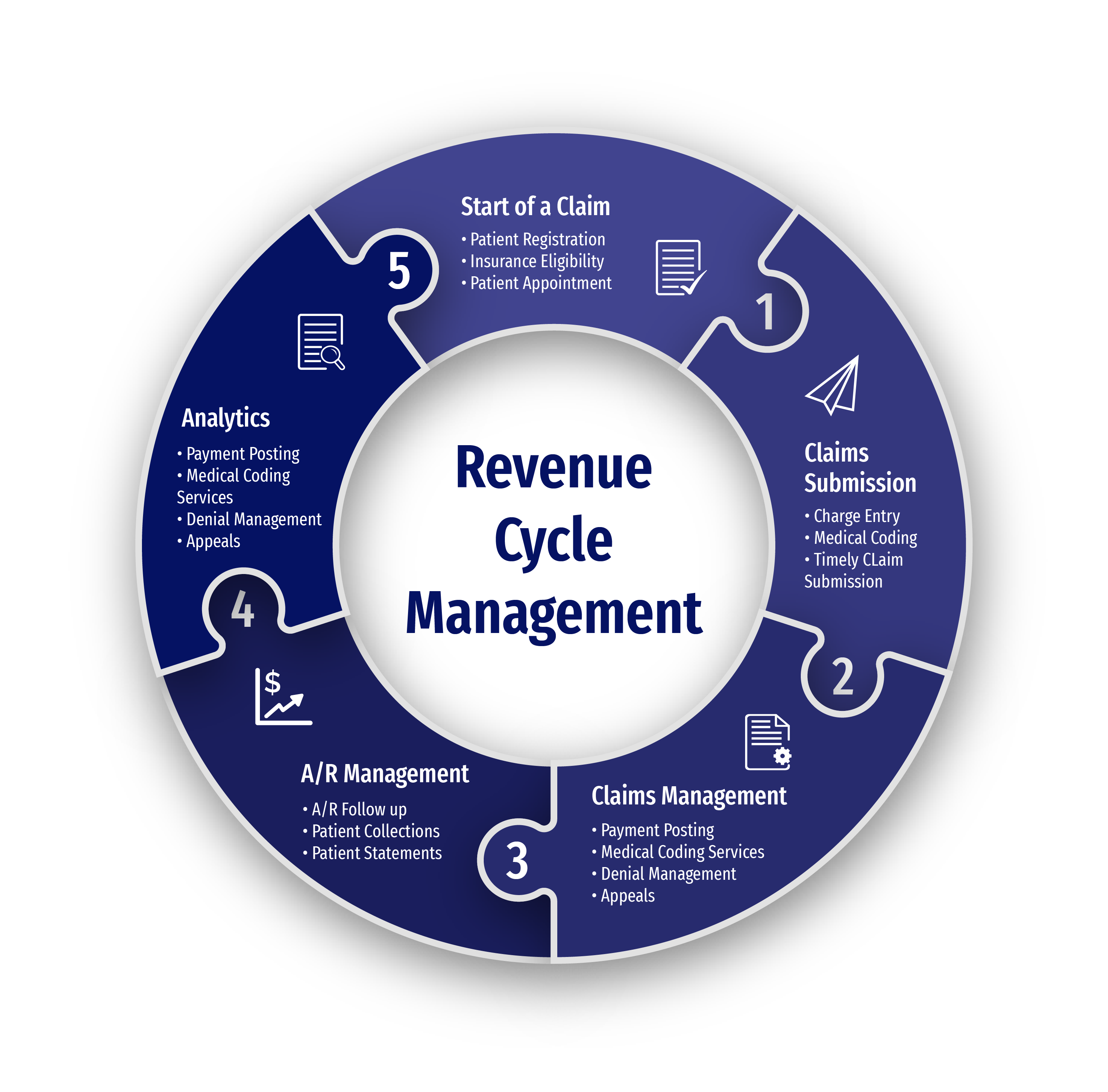
By partnering with us, you can streamline your revenue cycle management, reduce administrative burdens, and focus more on patient care. Our comprehensive behavioral health billing solutions cater to the diverse needs of behavioral health practices, ensuring compliance with industry standards and maximizing revenue.
Key Services
We are here to provide behavioral health billing services, ensuring a smooth operational workflow. Here's what we can assist with:
Appointment Scheduling
Patient Registration
Insurance Verification
Charge Entry
Claim Status and Follow-up
Payment Posting
AR Management
Rejections
Denial Management
Benefits of Outsourcing with Us
Cost Effective Support
Access remote healthcare back office support at competitive rates, ensuring increased cost-savings.
Operational Efficiency
Optimize your budget with streamlined processes and reduced overhead costs, allowing for efficient resource allocation.
Scalability Option
Quickly upscale healthcare operations without the burden of hiring and training additional staff.
Dedicated Team
Count on a team assigned to your healthcare organization, providing tailored support according your operational policies.

Why Use Our Behavioral Health Billing Services?
Specialized Expertise
Our team of billing professionals is well-versed in the intricacies of behavioral health billing. We understand the specific coding and documentation requirements needed to ensure accurate claims processing and reimbursement. With our expertise, you can trust that your billing is in capable hands. Our specialists keep up with the latest trends and updates in the field to provide the best service possible.
Improved Cash Flow
Efficient billing processes and prompt claim submissions are at the core of our services. By minimizing claim denials and optimizing revenue capture, our Behavioral Health Billing Solutions help improve the financial health of your practice, ensuring a steady and predictable cash flow. This allows you to reinvest in your practice and enhance the quality of care provided to your patients.
Accuracy and Compliance
Accuracy and compliance are paramount in behavioral health billing. We ensure that all claims are coded accurately and submitted in compliance with industry regulations, reducing the risk of claim denials and audits. Our team stays updated with the latest billing guidelines to ensure your practice remains compliant. We also conduct regular audits to catch and correct errors before they become an issue.
Cost-Effective Solutions
Outsourcing your billing to us offers significant cost savings compared to managing billing in-house. By eliminating the need for dedicated billing staff and software investments, you can reduce overhead costs and enhance your practice's profitability. Our transparent pricing models provide excellent value for your investment. These savings can be redirected to other critical areas of your practice.
Tailored Solutions
We understand that every behavioral health practice has unique needs. That's why we offer customized billing solutions tailored to your specific requirements. Whether you are a solo practitioner or part of a larger group, our personalized services ensure optimal results for your practice. Our team works closely with you to develop strategies that align with your practice's goals.
Focus on Patient Care
By outsourcing your billing to a behavioral health billing company like CLICKVISIONBPO, you can free up time and resources to focus on what matters most—providing quality care to your patients. Our comprehensive billing services handle the administrative burden, allowing you to dedicate more time to your patients' well-being. This enhances patient satisfaction and improves overall practice efficiency.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Other Specialties We Excel In
Psychiatry Billing Services
Psychiatry focuses on diagnosing and treating mental health disorders. Our Psychiatry Billing Services are tailored to support practices in handling claims for therapy, medication management, and psychiatric evaluations. These services complement behavioral health treatment by providing targeted care for various psychiatric conditions.
Neurology Billing Services
Neurology deals with disorders of the nervous system, including the brain and spinal cord. Our Neurology Billing Services simplify billing for diagnostic tests, treatments, and neurological consultations. These services often intersect with behavioral health, addressing conditions that may affect both mental and physical health.
Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Yes, part of our comprehensive behavioral health billing services includes thorough denial management. We investigate the reasons for claim denials, correct any issues, and resubmit claims promptly. Our team also reviews underpayments to ensure you receive the correct reimbursement for your services.
We prioritize the security and confidentiality of patient data. Our company adheres to strict HIPAA compliance standards, utilizing advanced encryption methods and secure access controls. Regular security audits are conducted to maintain the highest levels of data protection.
Yes, we offer customized billing solutions tailored to the unique requirements of each ophthalmology practice. Whether you need full-service billing or specific support in certain areas, we work closely with you to develop a personalized plan that meets your specific needs and goals.
Accuracy is ensured through our rigorous quality control processes. Our experienced billing professionals meticulously review and code each claim, adhering to the latest industry standards and regulations. Additionally, our internal quality control team double-checks all claims before submission to minimize errors and ensure compliance.
