- Home
- »
- Specialties
- »
- Cardiology Billing Services
Cardiology Billing Services | Cardiology Billing Company
Cardiology is a specialized medical field focused on diagnosing, treating, and managing disorders of the heart and blood vessels. From routine check-ups to advanced procedures like angioplasty and cardiac surgeries, cardiology plays a vital role in patient care. With the complexity of cardiovascular services comes the need for precise and efficient billing processes.
Our cardiology billing services streamline the billing process, ensuring accurate claims submission, timely reimbursements, and compliance with regulatory requirements. As a trusted cardiology medical billing company, we help practices focus on patient care while optimizing their revenue cycle.
Tailored Cardiology Billing Solutions
Our cardiology medical billing services address the unique challenges of cardiovascular practices. We provide:
Diagnostic Procedure Billing
Cardiology involves numerous diagnostic tests, such as ECGs, stress tests, and echocardiograms. We ensure accurate coding and documentation for these procedures, maximizing reimbursements.
Surgical Procedure Billing
From pacemaker insertions to open-heart surgeries, we handle the complex billing for surgical interventions, ensuring compliance with payer-specific requirements.
Cardiac Catheterization
Cardiac catheterization involves inserting a catheter into the heart to diagnose or treat cardiovascular conditions. Procedures such as right heart catheterization (CPT 93451) or left heart catheterization (CPT 93452) require precise coding and may involve multiple billing components, including professional and technical fees. Compliance with CMS guidelines is critical for reimbursement.
Cardiac Device Monitoring Billing
Billing for device monitoring, such as Holter monitors and implantable cardiac devices, requires precision. Our team specializes in handling these services to avoid payment gaps.
Claim Denial Management
Denials are common in cardiology billing due to coding errors or documentation gaps. Our proactive approach resolves denied claims swiftly to maintain your cash flow.
Pacemaker Implantation
Pacemaker implantation corrects heart rhythm abnormalities. Common CPT codes include 33208 for the insertion of a dual-chamber pacemaker. Billing challenges may arise when combining implantation with other procedures, requiring careful use of modifiers to avoid denials.
Benefits of Outsourcing Cardiology Billing Services
Expertise in Cardiology Billing
Our team has in-depth knowledge of cardiovascular procedures and payer requirements, ensuring accurate claims and maximized reimbursements.
Tailored Cardiology Billing
We customize our cardiology billing services to meet the unique demands of your practice, from routine diagnostics to advanced surgical procedures.
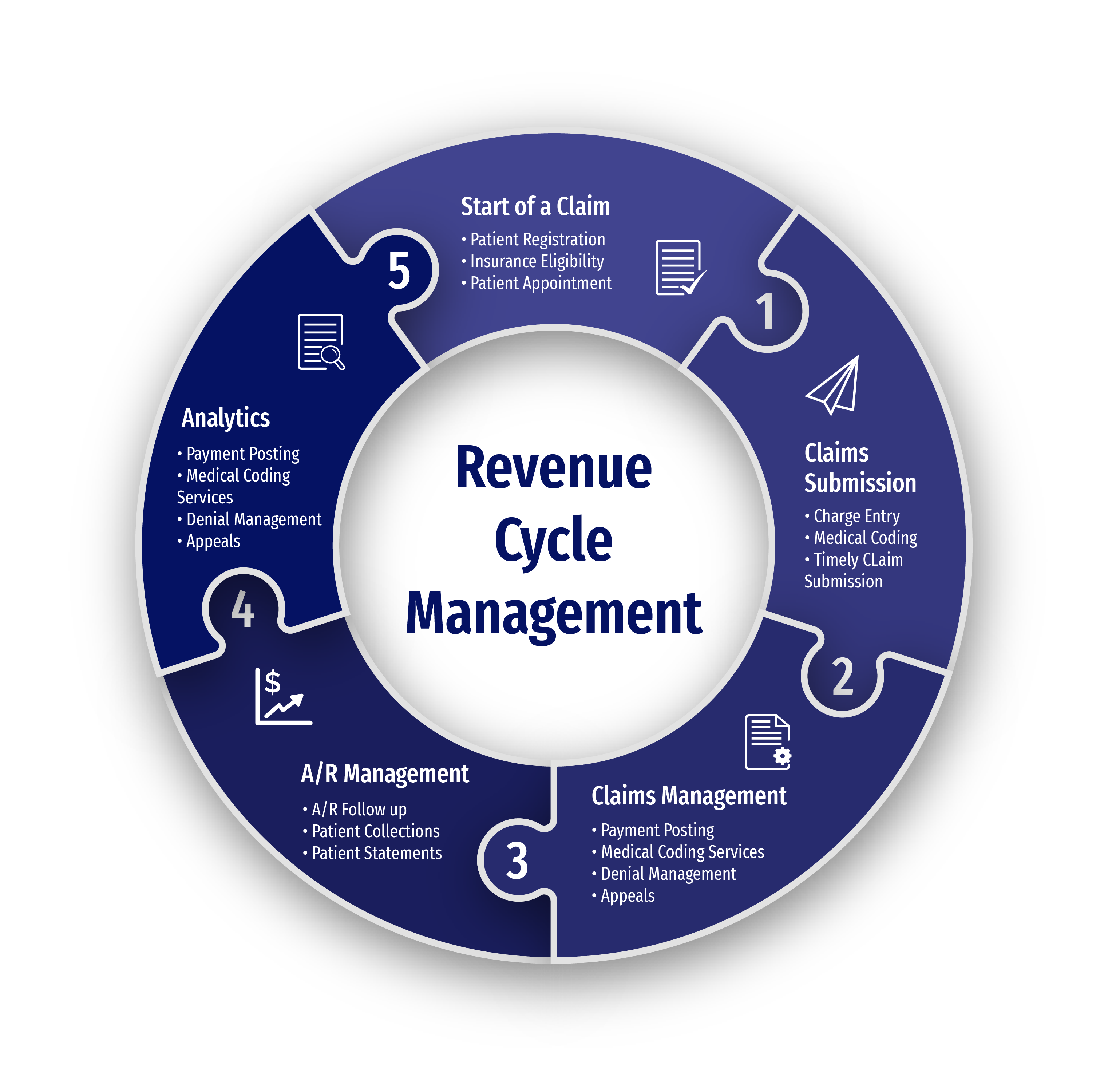
Improved Revenue Cycle Management
By outsourcing to our cardiology billing company, you ensure a streamlined revenue cycle, timely claims submission, and consistent reimbursements.
Reduced Administrative Burden
By choosing to outsource cardiology billing to us you allow your staff to focus on patient care, improving operational efficiency and patient satisfaction.

Cardiology Billing Challenges and Solutions
Complex Coding for Cardiovascular Procedures
Cardiology involves a vast array of diagnostic tests, interventional procedures, and treatments, each requiring precise coding to reflect the complexity of services rendered. Incorrect or incomplete coding can result in claim denials or reduced reimbursements, negatively impacting revenue. Our certified coders are well-versed in specific codes and maintain up-to-date knowledge of coding standards, ensuring compliance and minimizing errors.
Frequent Updates to Payer Policies
Insurance providers frequently revise policies, coverage criteria, and documentation requirements for cardiology services, making it challenging for practices to stay compliant. Missing even a minor update can result in rejected claims or revenue losses. We continuously monitor payer policy changes and align your claims with the latest requirements, ensuring seamless approvals.
Managing High Patient Volumes and Claims in Cardiology
With practices often handling numerous patients daily, the sheer volume of claims can overwhelm internal billing teams. Delays in claim submissions can disrupt cash flow and increase errors. Our team ensures timely and accurate claim submissions by streamlining the billing workflow, so your practice can focus on patient care.
Navigating Pre-Auths for Cardiology Procedures
High-cost procedures, such as angioplasty or cardiac imaging, often require pre-authorization to secure insurance approval. Obtaining these authorizations involves navigating complex payer protocols and can lead to delays in patient treatment. We manage the pre-authorization process from start to finish, ensuring approvals are secured promptly to maintain uninterrupted patient care and billing.
Resolving Denied and Underpaid Cardiology Claims
The intricate nature of cardiology services often results in claims being denied or underpaid due to documentation errors, miscoding, or payer discrepancies. These issues can cause revenue leakage if not addressed promptly. Our team conducts a thorough analysis of denied and underpaid claims, rectifies errors, and resubmits them to recover lost revenue effectively.
Ensuring Accuracy in Documentation and Compliance
Detailed documentation is critical for billing, as insurers often demand comprehensive records to justify claims. Inadequate or inconsistent documentation can lead to compliance issues and audits. We provide meticulous documentation support and ensure your practice adheres to all regulatory and payer guidelines, safeguarding your revenue and reputation.
Get In Touch
Send a message to discuss your specific needs and issues, and how we can assist you in solving them.
-
Send a Message
Share your requirements and challenges. -
Expect a Prompt Reply
Receive several solutions tailored to your needs. -
Schedule a Call
Arrange a discussion for further details.
Common CPT and ICD Codes in Cardiology Billing
Accurate cardiology billing relies on correctly linking CPT codes for procedures with their corresponding ICD-10 codes. This ensures proper claims processing and reduces denials. Below is a table of commonly used codes in cardiology to assist with compliant billing.
| CPT Code | Procedure/Service | Associated ICD-10 Codes | Description of ICD-10 Codes |
|---|---|---|---|
| 93000 | Electrocardiogram (ECG), complete | I10 | Essential (primary) hypertension |
| 93015 | Cardiovascular stress test, complete | I20.9, I25.10 | Angina pectoris, unspecified; Atherosclerotic heart disease |
| 93451 | Right heart catheterization | I50.9 | Heart failure, unspecified |
| 93458 | Coronary angiography with left heart cath | I25.110, I50.22 | Atherosclerosis with unstable angina; Chronic systolic heart failure |
| 93306 | Echocardiography (TTE), complete | R01.1, I51.9 | Cardiac murmur; Heart disease, unspecified |
| 93224 | Holter monitor, complete | I47.1, R00.2 | Supraventricular tachycardia; Palpitations |
| 92928 | Percutaneous coronary intervention (stent) | I25.10, I25.119 | Atherosclerosis of coronary artery; CAD with unstable angina |
| 33208 | Insertion of dual-chamber pacemaker | I44.2 | Atrioventricular block, complete |
| 33249 | Implantation of defibrillator system | I49.5 | Sick sinus syndrome |
| 93653 | Ablation therapy for arrhythmia | I48.91, I47.2 | Unspecified atrial fibrillation; Ventricular tachycardia |
Specialties We Excel In
Anesthesia Billing Services
Anesthesia plays a critical role in ensuring patient comfort during cardiology procedures, such as surgeries or diagnostic tests. Our Anesthesia Billing Services handle the complexities of billing for anesthesia administration, allowing cardiology practices to focus on patient care while we manage the associated claims.
Radiology Billing Services
Radiology is essential in cardiology for diagnosing heart conditions through imaging techniques like MRIs, CT scans, and X-rays. Our Radiology Billing Services simplify the billing process for imaging procedures, ensuring cardiology practices can efficiently manage diagnostic testing and integrate imaging with treatment plans.
Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
We provide wide range of medical billing services, including charge capture, coding, claim submission, payment posting, and denial management. Our comprehensive services cover all aspects of the billing process to ensure accurate and timely reimbursement for practices.
Outsourcing medical billing services to us can improve revenue cycle management by streamlining billing processes, minimizing claim denials, and accelerating reimbursement timelines. Our streamlined workflows and experienced team help practices optimize revenue and achieve financial stability.
Data security and confidentiality are crucial and we have rigorous measures to protect sensitive patient information. We have encryption protocols, access controls, and regular security audits to safeguard data against unauthorized access or breaches. Additionally, all team members undergo training on HIPAA compliance and adhere to strict confidentiality policies. We have a security measures policy document that can be requested for review at any time.
Our billing team makes a research to identify the reason for the denial. We then take appropriate actions to appeal the denial, resubmit the claim with corrections if necessary, and follow up with payers to ensure timely resolution. Our goal is to minimize claim denials and maximize reimbursements for our clients.
