- Home
- »
- Specialties
- »
- Internal Medicine Billing Services
Internal Medicine Billing Services
Internal medicine involves the diagnosis, treatment, and prevention of adult diseases, dealing with a wide range of conditions. As internal medicine encompasses a variety of medical specialties, it requires specialized billing solutions to ensure accurate coding and timely reimbursement.
Internal medicine billing involves precise documentation and coding of patient visits, procedures, and treatments tailored to the requirements of insurers and payers. Our internal medicine billing services ensure that your practice remains efficient, compliant, and properly reimbursed.
Our Internal Medicine Billing Solutions
We provide end-to-end billing support tailored for internal medicine practices, including:
Preventive Care Billing
Accurate coding for check-ups and health screenings for full reimbursement.
Chronic Disease Management
Efficient billing for diabetes, hypertension, and other long-term care.
Diagnostics & Lab Billing
Proper coding for lab tests and imaging to prevent denials.
Inpatient Care Billing
Detailed coding for hospital visits and procedures.
Follow-Up & Telehealth Billing
Streamlined billing for both in-person and virtual care.
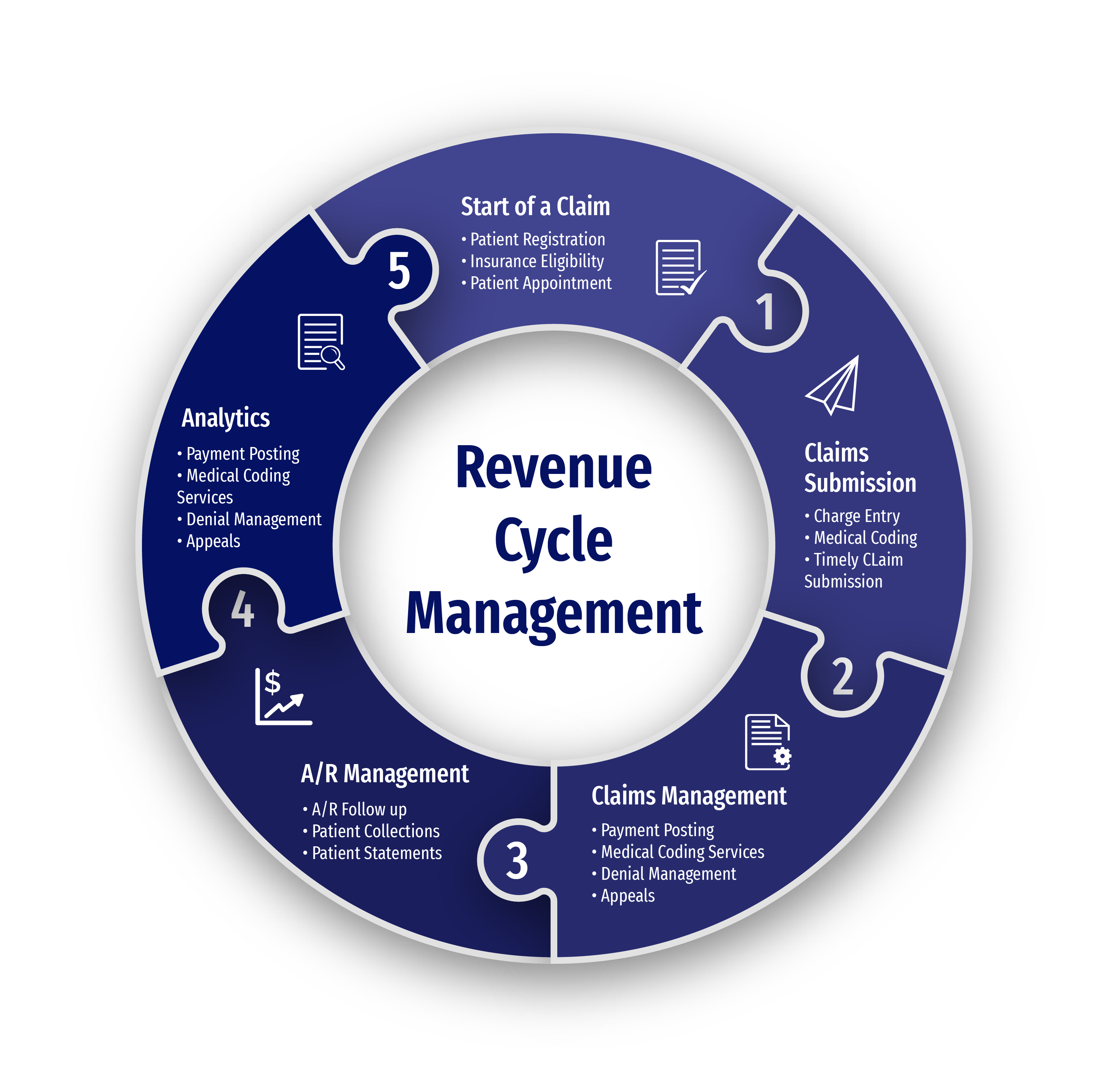
Our Internal Medicine Billing Services
Patient Registration & Insurance Verification
We ensure accurate patient data entry and real-time insurance verification to reduce claim rejections and confirm eligibility before each visit.
Accurate Coding & Claims Processing
Our certified coders apply precise CPT and ICD-10 codes for internal medicine services — including preventive care, chronic disease management, and diagnostic testing — ensuring clean, first-pass claims submission.
Payment Processing & Reimbursements
We post payments promptly, reconcile EOBs, and follow up with payers to accelerate reimbursements and maintain consistent cash flow.
Denial Management & AR Recovery
Our billing team identifies and corrects claim denials, manages resubmissions, and recovers outstanding balances to reduce aging accounts receivable.
Compliance & Documentation Review
We maintain full compliance with HIPAA, MACRA, and MIPS requirements, ensuring your billing practices meet the latest industry and payer regulations.
Common Internal Medicine Conditions We Bill
| Condition | CPT | ICD-10 |
|---|---|---|
| Hypertension | 99201–99215 | I10 |
| Type 2 Diabetes | 99201–99215 | E11 |
| COPD | 94664 | J44.9 |
| Hyperlipidemia | 80061 | E78.5 |
| GERD | 43239 | K21.9 |
| Anemia | 85025 | D64.9 |
| Depression | 99201–99215 | F32.9 |
Benefits of Outsourcing Internal Medicine Billing
Specialized Expertise
In-depth knowledge of internal medicine billing.
Improved Cash Flow
Faster reimbursements and fewer denials.
Regulatory Compliance
Adherence to HIPAA, MACRA, and MIPS.
Comprehensive Support
From insurance verification to denial resolution.

Internal Medicine Billing Challenges and Solutions
Complex Coding for Multidisciplinary Care
Internal medicine involves diverse conditions like hypertension, diabetes, and COPD, requiring precise coding under ICD-10, CPT, and HCPCS standards. Our team ensures accurate documentation and claims submission to reduce errors and maximize reimbursement.
Staying Compliant with Payer Policies
Insurance policies for preventive services and chronic care (e.g., diabetes management, health screenings) often change. We track updates from Medicare, Medicaid, and private insurers to ensure compliant claims, adhering to HITECH Act, MACRA, and MIPS guidelines.
Managing Claims for Preventive Services
Preventive services like wellness exams and vaccinations require correct coding to avoid denials. We ensure these services meet CPT and ICD-10 guidelines for timely reimbursement and eligibility for Meaningful Use incentives.
Leadership Team
Dimitar Talevski
Dimitar is a seasoned marketing specialist and the visionary behind CLICKVISION. With over 10 years in digital marketing, he excels in crafting marketing strategies that boost rankings, which in return increase leads, conversions, sales, profits, and ROI.

Filip Dimitrijevski
With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO's sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.

Help center
Got a question?
Get your answer
Quick answers to questions you may have about our internal medicine billing services. Can't find what you're looking for? Get in touch with us.
We reduce errors, boost reimbursements, and free your team from administrative burdens.
We specialize in internal medicine billing with a proven track record of compliance and accuracy.
By speeding up reimbursements, reducing denials, and maintaining consistent claim accuracy.
Yes — we follow HIPAA, MACRA, and other federal compliance standards.
