Plastic surgery billing is perhaps one of the trickiest processes in healthcare revenue cycle management. It requires extensive knowledge and experience so the claim can be submitted to the right payor. Following plastic surgery billing guidelines is essential for timely reimbursement, avoiding rejected claims, and staying compliant with the latest government and policy regulations.
The uniqueness of plastic surgery makes it a challenging field for billing. As very few plastic surgery procedures are covered by insurance, keeping up with the latest updates and understanding insurance policies is key. As medical billing experts, let us simplify the process for you so you can ensure financial stability.
Understanding Plastic Surgery Billing Guidelines
Plastic surgery billing guidelines ensure that healthcare providers receive timely reimbursement for the services rendered. It ensures proper documentation and compliance with the latest government and policy coding and billing regulations. In addition, by following these plastic surgery billing practices, your organization can improve its revenue cycle management. Following these guidelines ensures transparency, informs patients and insurance carriers about procedure expenses, and contributes to the provider’s financial stability.
Plastic surgery billing presents unique challenges, starting with complex coding requirements. Each type of service, such as surgical procedure, anesthesia, and post-operative care, must be properly coded and documented.
Other complexities associated with plastic surgery billing are insurance coverage limitations and violation of regulatory requirements and ethical standards regarding billing and coding.

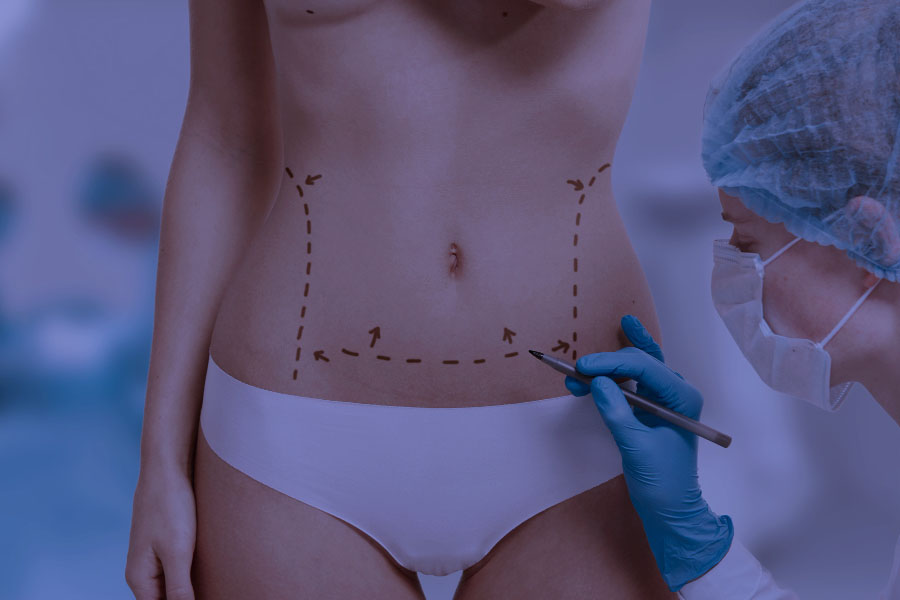
Cosmetic vs Reconstructive Plastic Surgery
Cosmetic or plastic surgery is defined as a procedure for improving the appearance of the patient by reshaping their normal body structures. According to the IOM 100-02 Chapter 16, cosmetic surgery expenses are not deemed a medical necessity and are generally not covered by insurance. Instead, they are typically billed to and paid by the patient.
Exclusions are certain surgeries that are considered reconstructive. Reconstructive surgery is defined as a procedure done on abnormal structures of the body that are a result of infection, tumor, disease, congenital defects, trauma, and developmental abnormalities.
Procedures that might be covered by insurance carriers
The American Association of Plastic Surgeons has published a list of plastic surgery procedures, that might be considered both cosmetic and reconstructive. Such procedures are:
| Cleft lip and palate surgery | Breast reduction for deformities that are not related to cancer treatment |
| Nasal surgery | Reconstruction after prophylactic mastectomy |
| Reduction mammaplasty | Nerve decompression for migraine surgery |
| Blepharoplasty | Skin lesions |
| Breast implant-associated anaplastic large cell lymphoma | Surgical treatment of obese and massive weight loss patients |
| Panniculectomy | Breast reconstruction after breast cancer treatment |
| Abdominoplasty | Ear deformity surgery |
Medicare has also published a short list of hospital outpatient services that might be considered cosmetic and covered by them:
- Blepharoplasty to remove the droopy excess tissue on the eyelid
- Botulinum toxin injections, known as botox, when it is used to treat muscle disorders such as spasms and twitches
- Panniculectomy for removing excess skin and tissue of the abdomen
- Rhinoplasty
- Vein ablation for closing off veins
Documentation Requirements
You must attach relevant documentation about the patient and the services provided to support the claim submission. Accurate documentation is required for compliance and timely reimbursement from the payor, whether it is the patient or the insurance company.
The documentation required for effective plastic surgery billing includes:
- Patient’s personal information
- Insurance details
- Medical history
- Record of cosmetic concerns
- Physical examinations
- Preoperative evaluations
- Surgical procedures performed
- Postoperative care
- Follow-up visits
Coding Excellence
The reimbursement process for plastic surgery procedures entirely depends on the coding and billing process. One of the most common reasons for claim denials is coding errors. Hence, accurate coding in plastic surgery and appropriate selection of CPT, ICD codes, and modifiers is necessary.
With medical coding, diagnosis, procedures, and medical services are translated into universal codes. The codes can be numerical, alphabetical, or a combination of both. CPT codes are used for translating services, while ICD-10 codes are for diagnoses.
CPT codes for plastic surgery
The table below contains the basic CPT codes related to plastic surgery.
| Codes type | CPT code number |
| Adjacent tissue transfer (skin grafts and flap procedures) | 14000 – 14302 |
| Myocutaneous flaps | 15570 – 15758 |
| Oral, facial and maxillofacial reconstruction | 21120 – 21296 |
| Rhinoplasty/nasal reconstructive surgery | 30400 – 30520 |
| Cosmetic procedures | 11950 – 17380 |
Every medical biller must be aware of and work according to the latest changes in plastic surgery medical billing. Failure to do so might result in increased denied claim rates. As a reference, only in the latest CPT annual updates, 230 new codes were introduced, 70 revised, and 49 were deleted. Modifiers were also updated, replacing the time ranges with a single total time amount.
ICD codes for plastic surgery
Regarding the coding system from the World Health Organization, the ICD-10 codes Z41.1 and Z42 are used for plastic surgery. Z41.1 is used for cosmetic surgery, while Z42 is used for reconstructive and plastic surgery following a medical procedure or healed injury.
In our experience, procedures that are coded Z41.1 are not covered by insurance carriers, while for some Z42 procedures, insurance might cover the costs.
Verification of Insurance Benefits and Pre-Authorization
Verification of insurance benefits is a process with significant importance for plastic surgery billing. With it, you, as an insurance provider, verify the insurance details of the patient and check whether they have adequate coverage for the reconstructive surgery.
Plastic surgery is one of the rare medical specialties that specifically requires prior authorization for almost every procedure. As a plastic surgery provider, you are obligated to send a pre-authorization request and proper documentation to the insurance carrier before performing the procedure.
Typically, if the insurance company approves the plastic surgery, it will cover part of the service amount, while the patient will need to pay the deductible or coinsurance. With pre-authorization, not only do you, as a service provider, ensure the plastic surgery will be covered, but you can also timely inform the patient about any out-of-pocket costs.
Claim Submission Process and Denial Management
The claim submission process for plastic surgery involves several steps. Typically, it starts with gathering the needed documentation and filing for pre-authorization. Also, explaining how the procedure is medically necessary might increase the chances of having the insurance carrier cover some of the costs.
The claim submission process continues with accurately entering the CPT codes and ICD in the system. Once the charges are accurately entered, you should check the created claim, and if everything is accurate, submit it to the payor. The best practice is to use electronic billing systems to submit the claim with all necessary documentation. Ensure you submit the claim within the deadlines set by the insurance company.
As we previously discussed, only specific plastic surgery procedures can be covered by insurance companies. Conseqnetly, having a denial management strategy in place is recommended for every plastic surgery provider. Some of the ways you can minimize rejections and maximize your revenue include:
- Keeping up with the latest regulations
- Timely claim submission
- Knowing when to submit a claim to the insurance company
- Analyzing and identifying common denial trends
- Understanding the reason for denials
- Attaching proper documentation to the claim
- Timely appealing denials
- Improving the coding and billing process and taking measures to prevent future denials
Outsourcing Solutions
Navigating plastic surgery billing effectively is not easy. Managing an in-house medical coding and billing team requires a lot of time and resources.
If you don’t have extensive knowledge about medical coding and billing and want to cut down your expenses and take off a huge administrative burden, you can always outsource. In fact, the number of plastic surgery departments and practices that outsource their medical coding and billing is rapidly growing.
By using CLICKVISIONBPO’s plastic surgery billing services, you gain access to an extraordinary team of responsible, educated, and experienced virtual medical billers and coders. We can streamline your entire revenue cycle management, maximize your revenue, and minimize your denial rates.
Conclusion
Adherence to plastic surgery billing guidelines ensures compliance with the latest regulations and might speed up the reimbursement process. In plastic surgery billing, it is of significant importance to distinguish between cosmetic and reconstructive procedures. This will ensure the claim is submitted to the right payor and reimbursed properly.If you want to improve your revenue cycle management, our CLICKVISION BPO team is here to create a tailored outsourcing medical billing strategy and efficiently manage your coding and billing needs. Contact us and let us handle everything for you with professionalism and transparency.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
