In the intricate landscape of healthcare reimbursement, the CMS plays a vital role in setting standards and regulations. However, the diverse CMS forms are core elements within this regulatory framework, documenting claims and seeking reimbursement for medical services. But what is CMS 1500 in medical billing, and what makes it so important?
Below, you’ll learn all about it!
What Is CMS in Medical Billing?
In medical billing, CMS stands for Centers for Medicare & Medicaid Services, which is vital in setting standards and regulations for healthcare reimbursement processes. Established under the Department of Health and Human Services (HHS), CMS ensures efficient administration of major medical care programs and health insurance exchanges like:
- Medicare – Manages coverage for individuals with disabilities, particularly those with end-stage renal disease (ESRD) and seniors ages 65 and above. CMS coverage can also benefit low-income families, pregnant women, and people who need long-term care.
- Medicaid – This is funded and managed by both state and federal governments and ensures low-income patients can easily avail of Medicaid coverage, offering a spectrum of healthcare services tailored by individual states.
- CHIP – Regulated by the CMS, the Children’s Health Insurance Program is designed to provide health access for children from low-income families, providing essential medical and dental care to enhance children’s well-being across the nation.
With a focus on improving overall health outcomes, access to coverage, and improving medical care quality, CMS is the foundation of healthcare systems. Through these programs, CMS endeavors to bolster healthcare accessibility while setting standards and regulations to uphold integrity and combat fraud.

Source: freepik.com/ Photo Contributor: jannoon028
What Does CMS 1500 Stand for in Healthcare?
To understand the intricacies of medical billing, you’d also require familiarity with the CMS 1500 form. So, what is CMS 1500 in medical billing?
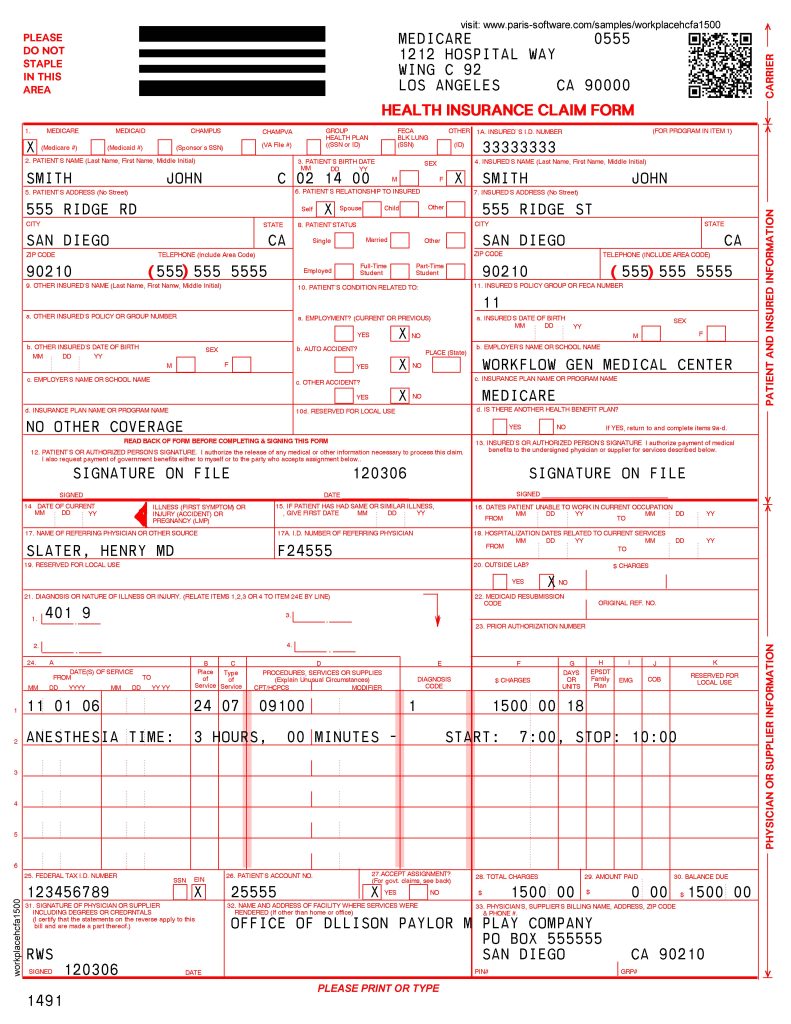
The CMS 1500, or HCFA 1500, is a crucial standard claim submission document utilized by healthcare providers and suppliers for billing Medicare and Medicaid. It is a vital tool in the health reimbursement process, ensuring accuracy and transparency in service descriptions for effective billing.
This document facilitates communication between insurance companies and healthcare providers, acting as a legal contract outlining the services to be provided. Thus, accurate completion and adherence to effective billing procedures are imperative for prompt payment and minimizing claim denials. This makes thorough understanding and training essential to avoid reimbursement delays and administrative burdens.
Moreover, this form is utilized by a diverse array of healthcare providers. It includes the following:
- Physicians and Specialists
- Non-Institutional Providers
- Surgeons
- Physical therapists
- Chiropractors
- Outpatient clinics
So, they all rely on the CMS 1500 to bill people for various medical services. From consultations and patient evaluation to minor surgeries, treatments, and post-operative care, this claim is a standardized means for accurate documentation when seeking reimbursement from insurers.
Key Components of CMS 1500 Forms
Before filling out the CMS 1500 forms, healthcare providers and billing staff must comprehensively understand its key components. Each of the 33 fields within the document serves a distinct function, including crucial details like patient demographics, provider information, service details, diagnosis codes, and procedure codes.
So, familiarity with these components ensures accurate form completion and minimizes errors and denials. Our expertise in handling claims and submissions while adhering to effective billing procedures can ensure prompt payments and minimize claim denials, reducing administrative burdens for healthcare providers. We’ll examine some of the most significant fields within the CMS 1500 and what they encompass, including:
- Field 1 – Details the patient’s health insurance type.
- Field 2 – States the patient’s complete name.
- Field 17 – Asserts the name of the referring healthcare practitioner if they referred the patient.
- Field 21 – Elaborates on the primary diagnosis code and the nature of the injury code.
- Field 24A – Contains the date that the medical service was rendered.
- Field 24G – Includes the number of days or units for the medical service rendered.
- Field 24I – Has the address and location of the medical service.
- Field 24J – Contains the ID number of the healthcare provider rendering medical services.
Submission Process for CMS 1500 Forms
For the claim to be processed and paid accurately, correctly, and completely, filling out the CMS 1500 forms is crucial. So, to ensure accurate and timely compensation, the following guidelines will help you navigate the process.
When filling out the CMS 1500 form, start by providing detailed patient information like name, birth, and contact details. Proceed to input insurance information, such as group or policy numbers. Then, fill in the diagnosis codes in sections 18-23, ensuring the inclusion of additional claims and outside lab information.
Next, specify the date and place of service in sections 24-30, aligning them with the services rendered. Complete the CMS form by detailing the medical care provided and corresponding CPT or HCPCS codes. Finally, ensure both patient and provider sign and date the document for authentication.
Submission options
Submitting the CMS 1500 form to insurers can encompass several options, including:
- Electronic submission methods streamline claim submission processes, allowing providers to send documentation directly to payers electronically, reducing processing time and potential errors.
- Clearinghouse services serve as intermediaries, validating and formatting claims before submitting them to insurers electronically.
- Paper submission options are the traditional methods of claim submission that involve mailing complete CMS 1500 forms to insurance payers.
While each method serves the same purpose, its diversity caters to the preferences and capabilities of individual healthcare providers and insurers alike.
Source: uslegalforms.com
Benefits of Using CMS 1500 Forms
Using CMS 1500 forms is an ideal method for providers seeking seamless reimbursement from insurers for their services in healthcare billing. As these documents are vital channels for communication between healthcare practitioners and insurance companies, optimizing their use is crucial for timely and accurate payments.
Beyond CMS 1500 forms’ advantages for streamlining the billing process and claim submission, they also offer:
- Standardization for effortless billing, providing a universally recognized structure for complex healthcare billing processes. Through CMS 1500, providers can achieve a streamlined approach, enabling them to easily navigate billing procedures.
- Comprehensive data collection for complete documentation is exemplified through the CMS 1500 form. It meticulously gathers patient data like diagnoses, procedures, and changes incurred as provider information, ensuring a detailed account of healthcare services and leaving no room for confusion.
- Seamless claim adjudication for swift payments relies on the CMS form. With detailed information, insurance companies can efficiently validate claims, expedite payments for practitioners, and provide timely and appropriate reimbursement.
- Accuracy in tracking and reporting services rendered through the CMS 1500 form extends beyond medical billing. It also offers valuable insight for tracking, reporting, and analysis, playing a crucial role in informing healthcare policies.
Regulatory Considerations for CMS 1500 Forms
When navigating the complexities of medical billing, ensuring adherence to healthcare regulations is vital for optimal compliance and accuracy. For example, they are HIPAA, CMS guidelines, and payer-specific requirements for claim formatting.
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law crucial in medical billing and set to safeguard sensitive patient health information. Proper compliance with HIPAA ensures that your organization handles private patient data on the CMS 1500 form securely and confidentially, preserving it from unauthorized access or disclosure.
Furthermore, CMS guidelines provide standardized protocols and procedures for billing processes, ensuring consistency, accuracy, and transparency. Adherence to these guidelines on CMS 1500 forms helps streamline billing processes and workflows, reducing the risk of errors or discrepancies that could lead to claim denials.
Lastly, payer-specific requirements refer to insurance companies’ unique formatting and documentation preferences. Providers must comply with the set demands to ensure that claims submitted on the CMS 1500 form meet each payer’s specifications.
Conclusion
So, what is CMS 1500 in medical billing? In conclusion, understanding and utilizing CMS 1500 forms are essential for efficient claim submission and reimbursement in the healthcare industry.
Proper completion and compliance ensure accuracy in billing practices, reduce the risks of errors, and facilitate timely payments and reimbursement from insurers. By leveraging the efficiency of CMS forms, your organization can uphold integrity in your billing processes and improve revenue cycle management, ultimately supporting the delivery of quality patient care.
We, at CLICKVISION BPO, offer comprehensive solutions tailored to navigate through the intricacies of medical billing.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
