The healthcare industry has always been held to strict rules and regulations that ensure patient safety and quality care. One safety factor that is vital in this process is provider credentialing. However, this element is often overlooked with many new businesses still learning about the standards and regulations. So, what is provider credentialing?
In this article, our expert team at CLICKVISION BPO will elaborate on the definition and importance of this process. We’ll also highlight the key components and steps within the credentialing process to help less experienced healthcare businesses understand them better.
Continue reading to discover all there is to know about provider credentialing, its process, and its importance!
Defining Provider Credentialing
Before we elaborate on the process, we first want to focus on the definition. So, what Is provider credentialing?
In simple terms, provider credentialing refers to a regulated process where healthcare organizations assess and verify the qualifications and licensing of specialized medical personnel. This includes various types of healthcare providers, such as nurses, physicians, physical therapists, and other allied healthcare providers. While provider enrollment is a related concept, it’s a different procedure. Enrolling a provider in a network involves registration of these verified providers with insurance companies and other payers.
Since these types of medical workers are responsible for specific patient services, they must undergo specialized training and certification. Thus, provider credentialing ensures the employees meet all the necessary standards and requirements to deliver safe and effective patient care.
The Significance of Provider Credentialing
While healthcare organizations need to conduct a background check on their medal providers’ information, competency, and skill levels, provider credentialing is also required by the Joint Commission on Accreditation of Healthcare Organizations and the Centers for Medicare and Medicaid Services. The main reasons why this process holds such significance within the healthcare industry are the following:
- Ensuring patient safety: Medical providers must have the training and qualifications to deliver safe and effective patient care. Thus, provider credentialing ensures the patient’s safety while reducing the risk of any medical errors.
- Ensuring care quality: By ensuring patients receive services from qualified and competent professionals, credentialing also upholds the standards of care within the healthcare industry.
- Regulatory compliance: As mentioned, regulatory bodies such as the Joint Commission and CMS require credentialing before they let someone practice medicine. So, your business must comply with these regulations to maintain its accreditation status and operate legally.
Key Components of Provider Credentialing
After discovering the definition and importance of provider credentialing, the next step is to elaborate on its key components. The ones that have the biggest impact on provider credentialing are the following:
- Background checks: Reviewing information for potential disciplinary actions or criminal history that may affect the employee’s suitability for practicing medicine.
- Education and training: The medical provider must have completed specialized educational courses from accredited institutions to provide suitable patient care.
- Specialty certificates: Ensuring the provider has the necessary specialized training or certifications to offer services in their specific field.
- Qualifications: Licensure verification to ensure the provider has a valid license in their field.
- Work history: Similar to many fields, working in the healthcare industry subjects the employees to employment history reviews. Hence, credentialing also delves into work history verification, such as relevant professional experience and past positions.
- Peer references: To ensure the provider’s adherence to professional standards and clinical skills, this process also involves gathering references from past employers, supervisors, and colleagues.
- Malpractice claim history: Often considered one of the most important factors of credentialing, the medical provider must have a spotless record regarding past professional and legal issues surrounding patient care.
Credentialing Process Overview
Now that you’re well-informed about the key components, we also want to give you an overview of the overall credentialing process. To better understand the process, we’ll highlight the most important steps. That being said, here is a detailed overview of provider credentialing:
- Gathering necessary data and documentation
- Verifying provider information
- Awarding the credentials

Source: freepik.com / Photo Contributor: gpointstudio
Gathering necessary data and documentation
The first step within the provider credentialing process is gathering the necessary data and documentation. During this primary phase, the credentialing apartment focuses on information gathering from multiple sources.
However, it’s important to mention that different insurance companies may require different documentation and forms. So, before you submit your application, it’s important to discover all the information the insurance company you plan to work with needs to prevent delaying the approval. Some of the most commonly required information during this process are the following:
- Name
- Social security number
- Demographic information
- Education
- Proof of licensure
- Career history
- Specialties
- Claim history
- Proof of insurance
- Information about the healthcare facility
Verifying provider information
After the necessary data has been gathered, the next step is to verify the provider’s information. Often considered the most time-consuming part of the process, all the documentation has to go through primary source verification to ensure its reliability. Any secondary sources can be easily falsified, providing outdated, inaccurate, or biased information.
The two main ways you can verify such data are manually or through the use of credentialing software. While the first option requires you to personally contact medical schools and other organizations to double-check the resume and board certification, the latter automates parts of the process by cross-referencing application and resume information with medical schools and AMA profiles.
Failing to verify the needed information can lead to missed malpractice claims and medical incidents that may put your patients at risk. Furthermore, it can lead to delays in the credentialing process, which can last from a few weeks to months.
Awarding the credentials
After all the documents and data have been verified, the provider will be awarded their credentials if everything is up to the required standards. Once this happens, the employee is granted clinical privileges and can practice medicine on-site.
However, it’s important to mention that even if all your documentation fits the necessary requirements, the approval length can last anywhere between 90 to 150 days. If any additional issues arise, the credentialing process can also be indefinitely prolonged.
Credentialing Standards and Regulations
Since provider credentialing is one way to ensure patient safety and quality services, there are specific standards and regulations it must oblige to. The ones that you should be especially mindful of are the following:
- Accreditation organizations: Healthcare organizations have to comply with the accreditation standards set by bodies like the Joint Commission and the National Health Service.
- Government regulations: If a healthcare facility participates in a government-funded healthcare program, then it will be subjected to a set of regulations provided by the Centers for Medicare and Medicaid Services (CMS).
- Professional associations: Depending on the healthcare discipline, your organization may have to follow credentialing standards set by the American Medical Association.
- State licensing boards: These bodies regulate the medical practice of any healthcare provider within their jurisdiction. They also establish licensure requirements associated with education and training.
- Insurance companies: Insurance networks have their own specific credentialing standards to align with the industry’s best practices and can involve licensures, education, and malpractice history.
- HIPAA compliance: Any type of credentialing process must comply with HIPAA (Health Insurance Portability and Accountability Act) regulations to ensure the safety of patient health data.
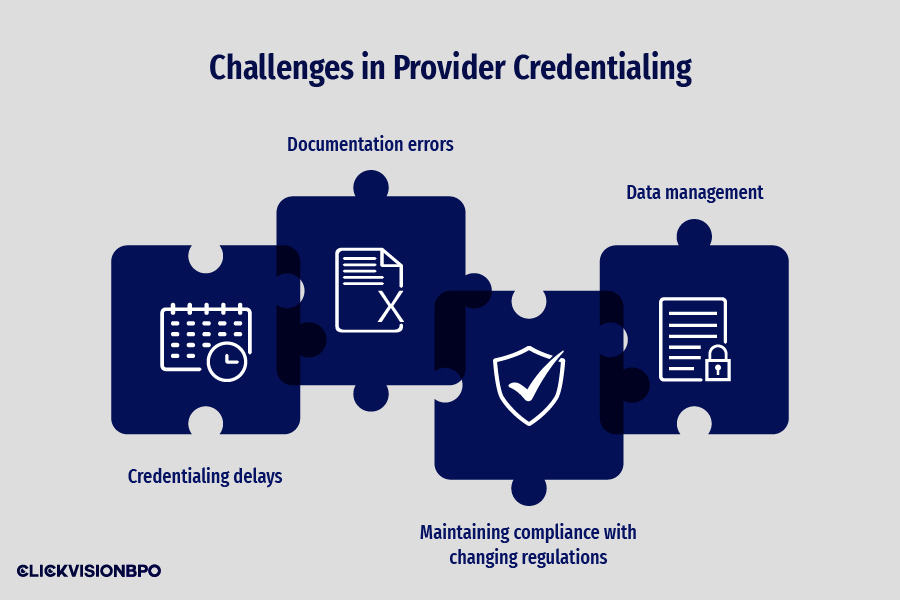
Challenges in Provider Credentialing
As with any business operation, provider credentialing has several challenges you should consider. To best prepare for this process, the main issues you should be mindful of are the following:
- Credentialing delays: One of the most common challenges in provider credentialing is the potential delay. Credentialing itself is a complex and time-consuming process that requires patience and attention to detail. Since it requires gathering and verifying large volumes of data, a normal process can take up to three months.
- Documentation errors: Another common problem that may arise during the credentialing process is the inability of the provider to provide all the necessary documentation. Such incomplete documentation can lead to further delays and even denials.
- Maintaining compliance with changing regulations: The healthcare industry is often subjected to changes as technology and patient services evolve. So, healthcare organizations have to keep up with the frequently changing regulations to maintain compliance.
- Data management: Provider credentialing deals with a large volume of personal and professional information. Hence, ensuring data accuracy and security can become quite challenging.
Importance of Ongoing Monitoring and Re-credentialing
Another important aspect we want to cover is the importance of ongoing monitoring and re-credentialing. The main reason why this process is crucial for healthcare organizations is to ensure continued competency and compliance over time.
Since medical providers are responsible for the lives and safety of their patients, they have to maintain their skills and knowledge throughout their careers to ensure high-quality care. Thus, ongoing monitoring is essential for performance evaluations to ensure the personnel’s continued competency.
Another reason why re-credentialing is important is that many regulatory and accrediting bodies ask healthcare organizations to release their employees’ credentials to ensure they oblige to the standards and regulations. This way, they can track the provider’s performance and identify potential malpractice and disciplinary risks. In most states, the re-credentialing process occurs every two years.
Additionally, the healthcare organization will minimize any financial and legal liabilities while ensuring the quality of its services. The last reason why this practice is important is because it proves to the insurance network that the provider is still eligible to participate.
Technology Solutions for Provider Credentialing
In today’s modern age, there has been an increase in technological advancements that aim to ease the credentialing process for healthcare organizations. While some focus on automating the verification process, others deal with data management. However, the main technology solutions that play a vital role in this process are the following:
- Automated verification: With access to primary source databases, credentialing software can validate qualifications from medical schools and boards. Besides the primary function to help healthcare organizations review the documentation manually, some options include features such as securely storing provider information and generating reports for compliance purposes.
- Electronic applications: With such application forms, providers can quickly submit their credentials to save time and minimize any chance of errors.
- Digital credentialing: With digital credentials such as badges and certificates, healthcare providers can easily share them with the required bodies online.
- Automated alerts and reminders: Many credentialing software can track expiration dates and alert the healthcare organization when it’s time for re-credentialing. Some may even give information about missing documentation and pending application statuses.
Conclusion
So, what is provider credentialing? After discovering what the process consists of, it’s important to emphasize its critical role in maintaining quality care and patient safety in healthcare settings.
Ensuring your healthcare providers have all the necessary training and qualifications is essential for legally operating your business. Often considered a complex and time-consuming process, it’s important to be mindful of the challenges and regulations credentialing is subjected to.
Hence, if you’re ever in need of specialized outsourcing credentialing services, contact our team at CLICKVISION BPO, and we’ll come up with the right solutions for your unique needs. Alongside our customizable services, we take pride in our perfectly tailored plans based on your requirements.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
