In today’s age, the medical industry is closely connected to the insurance sector. Healthcare organizations must be mindful of numerous requirements and standards to ensure they operate legally and generate revenue. One such process is known as enrollment, which plays a crucial role in medical billing. So, what is provider enrollment, and how does it affect the operations of healthcare facilities?
In this article, we’ll elaborate on the definition and use of this process while highlighting its key components. Since provider enrollment ensures that the healthcare providers get paid for their services, we’ll explain the process itself and focus on the benefits it offers. To better navigate this enrollment, we’ll discuss the common challenges you may face and elaborate on what differentiates it from medical credentialing.
Continue reading to discover all there is to know about provider enrollment and its importance in the medical industry!
What Is Provider Enrollment?
Before we elaborate on the use and importance of provider enrollment, we first want to define it. In simple terms, provider enrollment is the process of healthcare providers applying to become part of a specific health insurance network. Often referred to as payer enrollment, it’s how doctors, hospitals, and clinics get authorized and registered to participate in private and government medical programs.
If the enrollment is successful, then you’ll be considered an in-network provider, which comes with its own perks and benefits. However, the main reason why provider enrollment is vital to a healthcare organization is that its providers will be able to bill for the services they offer to patients that are covered by the specific program.
Since the plans vary depending on the program, it’s best to familiarize yourself with the procedures and requirements of the ones you’re interested in applying for. The most common options include Medicaid, Medicare, and many other private insurance networks.

Source: freepik.com
Key Components of Provider Enrollment
Now that we’ve covered the provider enrollment definition, we also want to elaborate on the key components the process consists of. The ones you should know before starting the application process are the following:
- Applications – As with any enrollment process, you’ll need to acquire the appropriate application forms and fill them with the necessary information. For healthcare providers, it’s important to include practice-related information, such as qualifications and credentials.
- Documentation – The enrollment process requires a large volume of paperwork to ensure the provider is eligible. Thus, it’s best to gather all the essential documentation beforehand, including licenses, diplomas, and other relevant credentials.
- Enrollment fees – Some programs you may be interested in also require payment. Whether it’s an enrollment fee or administrative costs, planning your budget beforehand is best.
- Verification – Since healthcare providers work with real-life people, all the submitted documentation must be verified to ensure patient safety and quality care. So, you should be prepared for background checks, which ensure compliance with legal and regulatory requirements.
- Revalidation – The provider may undergo periodic revalidation to maintain active enrollment status. In most cases, this process is required every 2 years to ensure the provider has continued compliance with the specific program.
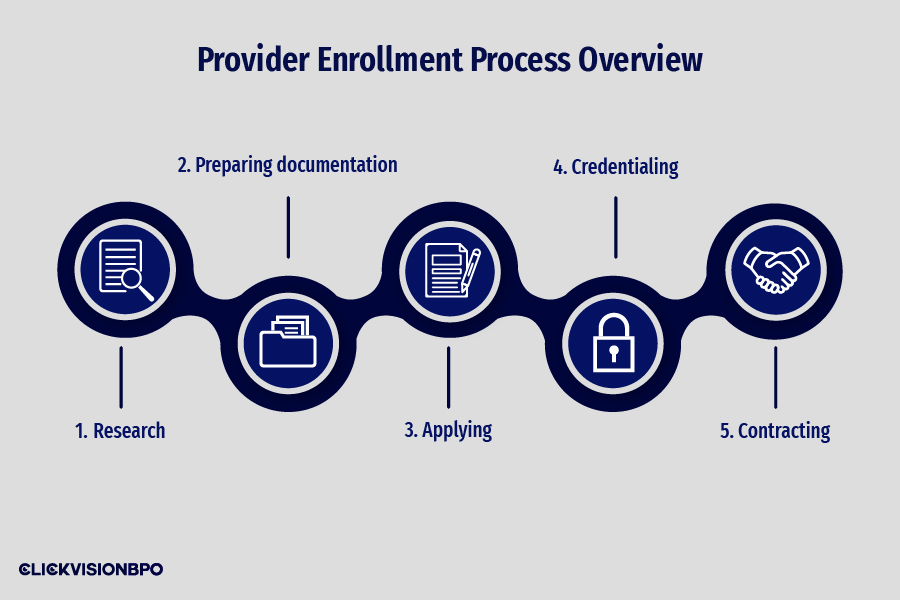
Provider Enrollment Process Overview
To ensure the enrollment process goes as smoothly as possible, it’s important to be mindful of several crucial steps. Here is a step-by-step provider enrollment process overview to better prepare you for your upcoming application:
- Research – Before you begin applying to healthcare programs, it’s important to take the time and research the plans and options they offer. This way, you’ll better understand the eligibility requirements set by Medicare, Medicaid, or your desired private insurance network.
- Preparing documentation – The next step is to gather all the needed documentation, including certification, licensure, and malpractice insurance.
- Applying – After gathering the necessary documents, you must complete and submit an application form.
- Credentialing – Often considered the most complex and time-consuming aspect of enrollment, provider credentialing is used to verify the competence of the healthcare provider. Since the process involves large volumes of paperwork for proof, preparing any licenses, certifications, tax and work records, and proof of insurance and immunization beforehand is best.
- Contracting – If the provider has been approved to join the program, they must negotiate a credentialing contract. Since it defines your reimbursement rates, it’s best to negotiate your rates before signing it and becoming their in-network provider.
Common requirements for provider enrollment
Even though you may have memorized the enrollment process itself, it’s also important to stay mindful of its common requirements. For a successful enrollment application, you’ll need to disclose the following information:
- Personal information – Includes the practitioner’s full name, contact information, address, driver’s license, and Social Security number.
- Licensure and certifications – You’ll need to provide copies of all currently active state licenses and certificates with expiration dates. This will be used as proof that the provider has the necessary training and education to practice medicine in their field.
- Professional experience and references – It’s important to include a detailed work history, including all practice locations and written letters of recommendation.
- Malpractice and disciplinary history – To ensure the provider is fit to practice medicine and provide quality patient care, you must submit detailed malpractice claims, third-party documentation for disciplinary actions, and a certificate of Professional Liability Insurance Coverage.
- Continuing education – It’s important for healthcare providers to keep track of the latest developments in the industry through Continuing Medical Education (CME) activities. Thus, you’ll need to provide proof of any workshops, conferences, or online courses the provider has taken part in.
Payer-specific enrollment requirements
Since the necessary documents may differ depending on the healthcare program you wish to apply for, we also want to cover some common payer-specific enrollment requirements you should know of. The ones that have the biggest impact on the overall enrollment process are the following:
- Enrollment fees – As mentioned, some healthcare programs have enrollment fees for your application. For example, both the Medicare and Medicaid programs have a $709 fee you have to cover before you apply to become part of their program.
- Professional identification numbers – These social identification numbers are used to describe the provider’s profession and degree of expertise. They can be issued by various regulatory bodies, such as government agencies, healthcare institutions, and professional organizations. The most popular identifier for this process is the NPI (National Provider Identifier), which needs to be included in the application for identification purposes.
- Credentialing criteria – Remember that each healthcare program has its own unique credentialing criteria you should meet. For example, the minimum work experience, education, and training may vary depending on the payer’s requirements.
Benefits of Provider Enrollment
So, why should you take the time to go through the provider enrollment process? As mentioned, healthcare organizations gain access to numerous benefits by having in-network providers.
- Increased patient access – With in-network providers, the healthcare organization gains access to a wider audience, meaning new patients. Furthermore, provider enrollment can also give you access to patients under the Medicare and Medicaid insurance programs alongside those with private insurance.
- Credibility and trust – Having in-network providers also builds credibility and trust within the community. By enrolling in reputable healthcare programs, you demonstrate compliance with their requirements and standards. By doing so, it showcases your capability to provide high-quality medical care and services that your patients can trust.
- Enhanced revenue opportunities – One of the main benefits of provider enrollment is the ability to bill for the services you offer to insurance-covered patients. Thus, you’ll be ensuring timely reimbursement for any medical services and treatments, leading to generating more revenue.
- Compliance with regulations – Since healthcare organizations are responsible for the well-being and safety of patients, they must oblige to a strict set of rules and regulations. This way, provider enrollment showcases your compliance with care standards, patient privacy, and billing practices.
Credentialing vs. Enrollment
Since we’ve noticed a lot of people confuse provider enrollment with credentialing, we want to highlight the aspects that differentiate the two. Even though both processes are related, their use and functions are different.
Medical credentialing is an important process for determining a provider’s competence in a specific field. This regulated process is used to verify the qualifications and licensing of healthcare providers, such as physicians, nurses, dentists, physical therapists, and other allied medical providers. Credentialing also ensures that the provider in question has the needed education and training to practice medicine and provide proper patient care.
On the other hand, provider enrollment deals with the registration of healthcare providers in insurance networks and healthcare payers. This way, the healthcare organization can participate in reimbursement programs and bill for the services they’ve offered to patients covered by the specific network they’re part of.
Even though both processes require you to submit an application, provide the necessary documentation, and go through background checks, provider enrollment also includes signing agreements or contracts with the chosen insurance network.
Navigating the Enrollment Process
Since provider enrollment may initially sound complicated, we want to help you navigate the process without any delays. With the experience we’ve gathered working in this industry, we want to share the best tips and tricks for a straightforward enrollment process. Here’s what you should focus on during your application:
- Proper documentation preparation – The first thing you should focus on before submitting your application is proper documentation preparation. For this step, it’s important to answer all questions in detail and provide relevant information that can be verified from the main source. While it may seem simple, improper paperwork is the main cause of delays and denials.
- Timely submission – Many healthcare programs have specific timeframes in which you should deliver all the necessary paperwork, such as the application, documentation, and enrollment fees. Respecting the deadlines helps the payers efficiently manage the enrollment process, preventing any delays. Furthermore, timely submission ensures the provider starts participating in the program as soon as possible.
- Communication with payers – Whenever you have any questions about the enrollment process and submission, we encourage you to contact your chosen healthcare program. Their enrollment department or contact person will clarify any misunderstanding and guide you for future queries.
Challenges in Provider Enrollment
As with any business operation, there are challenges in provider enrollment you should be mindful of. The two that have the biggest impact on your healthcare organization are the following:
- Application delays
- Credentialing discrepancies
Application delays
One of the most common challenges in provider enrollment is getting your application delayed due to issues in the paperwork you provide. As mentioned, both enrollment and credentialing are complex processes that deal with large volumes of documentation. So, any missing documents or information may prolong the already long wait for your application to get approved. While the typical wait time is approximately 90 days, such issues may indefinitely delay the process.
To ensure that the enrollment process is as straightforward as possible, gathering all the needed documentation beforehand is best. Since all the information has to be verified from the main source, always thoroughly review the paperwork to find any errors or missing data that may occur.
Credentialing discrepancies
The second common issue in provider enrollment is credentialing discrepancies. Depending on the program you want to enroll in, there are different requirements and documentation you need to be mindful of. Since the credentialing process is a common prerequisite for participating in a certain healthcare network, some programs have strict credentialing requirements you should familiarize yourself with beforehand.
Furthermore, even though you may have already submitted an application to the same program in the past, remember that the credentialing requirements change over time. This is mostly due to the evolving industry standards that encourage healthcare providers to adapt to the field and update their credentialing process accordingly. Thus, researching the specific and up-to-date rules and regulations of the program you’re interested in is a must if you want to get enrolled without any delays or denials.
Source: freepik.com / Photo Contributor: Drazen Zigic
Conclusion
What is provider enrollment? After elaborating on its use and importance, remember that this process is crucial for your healthcare organization to get paid for the services it offers.
Since we understand how complex it may be to navigate all the rules and regulations that come with running a healthcare facility, our team at CLICKVISION BPO has designed a new sector that focuses solely on meeting the diverse needs of the healthcare and insurance industries.
Our customizable services range from credentialing services to medical billing and coding. So, if you’re ever in need of outsourcing services ready to meet your diverse needs, contact our experienced team and discover how you can improve your healthcare operations!

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
