Medical Billing Services for Small Practices
Small practices face unique challenges in managing revenue cycles while delivering quality care. At CLICKVISIONBPO, we provide tailored medical billing solutions, including insurance verification, claims submission, and revenue cycle management (RCM).
Our expertise in ICD-10 coding, CPT codes, and payer-specific guidelines ensures accurate, compliant billing. Whether you’re a primary care provider or a specialized clinic, our HIPAA-compliant services help streamline operations and maximize reimbursements.
Our Medical Billing Services for Small Practices
Our medical billing services are tailored to streamline administrative workflows and enhance the financial performance of small practices. Below are the services we provide:
Insurance Verification
We verify patient insurance coverage and eligibility for treatments and procedures, ensuring accurate pre-authorizations. This reduces claim rejections and helps maintain a seamless revenue cycle for your practice.
Accurate Medical Coding
Our team specializes in ICD-10, CPT, and HCPCS Level II coding to accurately document diagnoses and procedures. This ensures compliance with payer-specific requirements and maximizes reimbursements.
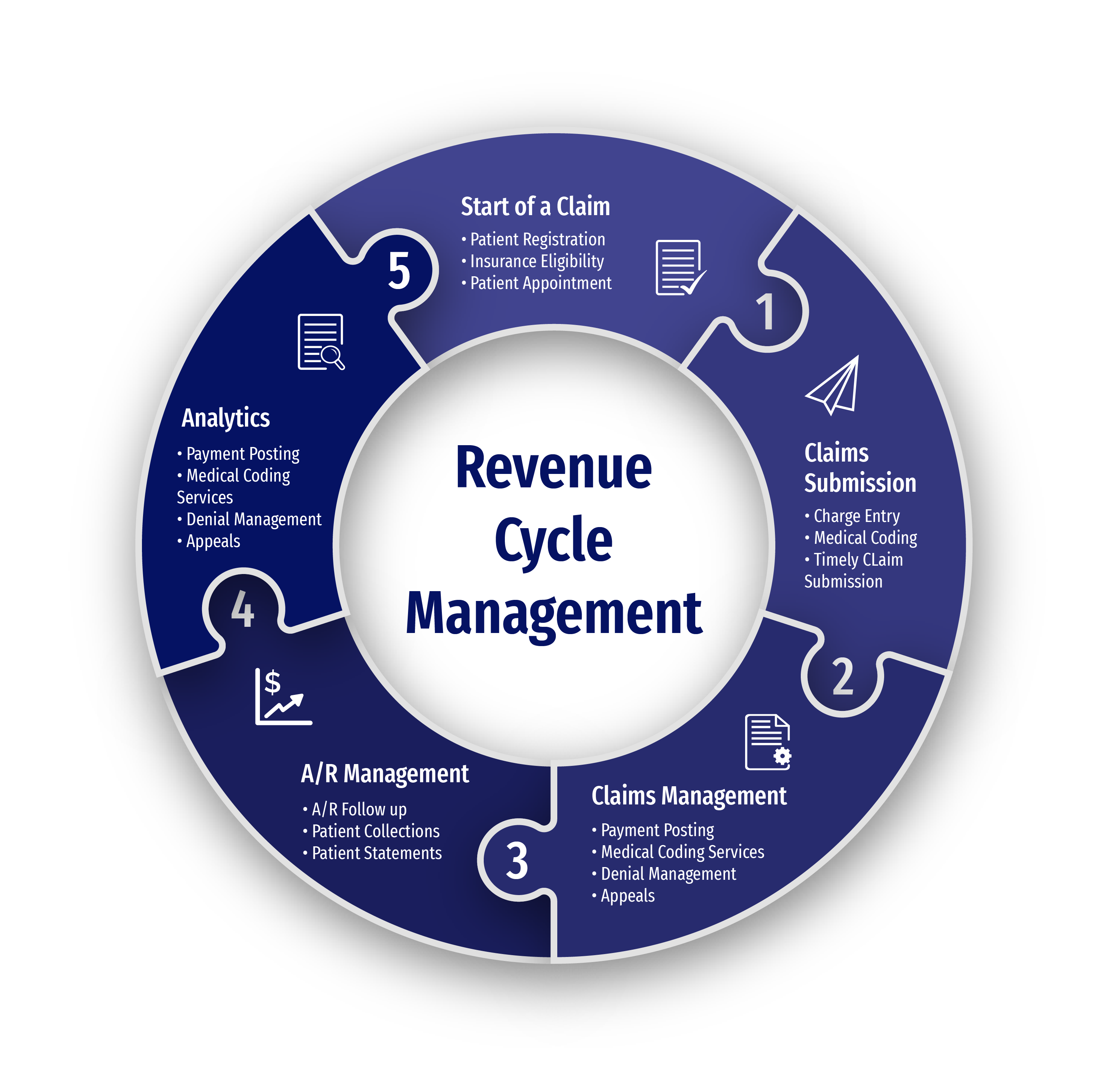
Revenue Cycle Management (RCM)
Our end-to-end RCM services address inefficiencies in billing workflows, optimize cash flow, and improve the overall financial health of your small practice through regular audits and process enhancements.
Claims Submission and Denial Management
We handle the timely submission of clean claims, reducing the risk of errors and delays. Our denial management process identifies and resolves issues quickly, minimizing revenue loss and ensuring efficient appeals.
Why Choose Us for Small Practice Billing?
At CLICKVISIONBPO, we offer specialized medical billing solutions that streamline your practice’s operations. Here are four reasons to partner with us:
Maximized Reimbursements
Our expertise in ICD-10, CPT, and payer-specific coding ensures accurate claims submission, resulting in faster approvals and higher reimbursements for your practice.
Tailored Solutions for Small Practices
We provide customized billing services for primary care and specialized practices, ensuring seamless integration with your workflow and maximizing efficiency.
Compliant and Secure Billing
We adhere to HIPAA and CMS guidelines, ensuring your practice’s billing process remains compliant, secure, and free from regulatory risks.
Cost-Effective and Scalable
Outsourcing your billing reduces the need for in-house staff, cutting overhead costs while maintaining a high level of service and scalability as your practice grows.

Challenges Small Practices Face
Complex Medical Billing and Coding
Small practices often face challenges in accurately using ICD-10, CPT, and HCPCS codes for a wide variety of treatments, from preventive care to specialized procedures. Incorrect coding can result in denied claims and delays in reimbursement.
Insurance Verification and Authorization Issues
The process of verifying patient insurance can be cumbersome and time-consuming. Prior authorizations, insurance eligibility, and coverage verification often cause delays in the billing process, affecting the practice’s cash flow and revenue cycle management.
Regulatory Compliance Challenges
Maintaining compliance with evolving healthcare laws such as HIPAA and CMS guidelines is a significant challenge. Small practices struggle with the complexity of federal regulations, payer-specific requirements, and state regulations, increasing the risk of costly errors and penalties.
Inconsistent Cash Flow
Delayed payments and frequent claim rejections often result in disruptions to the practice’s revenue cycle. Practices may find it difficult to manage cash flow, particularly with Medicare, Medicaid, and private insurance reimbursements that require detailed claims follow-up.
Time-Consuming Denial Management
Dealing with claim denials requires a deep understanding of payer policies, appeals processes, and medical billing procedures. Small practices often lack the resources to manage this process effectively, resulting in lost revenue and additional administrative burden.
High Administrative Burden
Small practices often face overwhelming administrative workloads, including billing, coding, claims submissions, and patient statements. This leaves little time for patient care and clinical operations, reducing overall efficiency and growth potential.
Industry Tailored Medical Billing for Small Practices
We work different specialties in medical billing. Here's a list what practices we can help:
Help center
Got a question?
Get your answer
Quick answers to questions you may have. Can't find what you're looking for? Get in touch with us.
Medical claims can be denied for several reasons, including incorrect coding, missing documentation, expired authorizations, or patient eligibility issues. It's essential to have a streamlined process for claims verification and coding accuracy to minimize the risk of denials.
The Healthcare Common Procedure Coding System (HCPCS) and CPT codes are regularly updated. Medical billing providers need to stay informed through resources such as American Medical Association (AMA) updates, CMS, and industry news to ensure accurate coding and billing practices.
Timely billing is crucial for maintaining a healthy cash flow in healthcare practices. Delayed claims can lead to revenue loss, increased administrative costs, and delayed reimbursements from insurance companies. Efficient billing practices ensure quicker approval and higher reimbursement rates.
Insurance verification ensures that patients' insurance details are accurate and up-to-date before services are provided. It is a critical step to confirm coverage and prevent issues with claim processing. This process helps prevent denied claims and unnecessary delays in reimbursements.
Medical billing services for small practices streamline billing processes, reduce administrative burdens, and improve reimbursement rates. By outsourcing to experts, small practices can ensure accurate coding, timely claim submissions, and efficient denial management, allowing healthcare providers to focus on patient care while optimizing revenue cycle management.
| Regulatory Body | Role in Medical Billing | Key Focus Areas |
|---|---|---|
| HIPAA | Ensures privacy and security of patient health information | Confidentiality of personal health information (PHI), prevention of data breaches |
| CMS | Sets standards for Medicare and Medicaid billing | Compliance with Medicare and Medicaid billing codes and processes |
| OIG | Prevents fraud and abuse in healthcare billing | Adherence to regulations to avoid fraud, particularly in Medicare and Medicaid |
| ANSI | Establishes standards for electronic healthcare transactions | Standardization of electronic claims and remittance advice |
| State-Specific Regulations | Ensures compliance with state healthcare laws | Adherence to individual state healthcare and insurance billing rules |
| NCQA | Improves healthcare quality through compliance and billing accuracy | Focus on efficient billing practices for better patient care and performance |
