In the past years, the healthcare industry has become more complex than we know it. Worse yet, organizations constantly face increasing pressure to deal with changes in policies and regulations. To effectively manage and navigate claim processing, organizations try to employ more efficient processing methods. That’s why it is important to understand what is claims management in healthcare and why it stands as a core element that every organization should optimize and prioritize.
With our help, organizations can seamlessly leverage the numerous benefits of effective claims management and reach unparalleled success and revenue generation!
Understanding Claims Management
Claims management refers to the comprehensive process of handling medical claims from submission to payment. It involves a systematic approach to organizing, filling, and processing claims related to medical services rendered, encompassing various stages such as reporting, investigation, evaluation, and settlement. With a robust claims management strategy in place, you can streamline processes, improve cost control, and enhance overall customer satisfaction.
However, the sheer volume of data that’s involved in claim management can be an overwhelming struggle for many organizations, demanding innovative solutions to efficiently handle and process information. That’s why many insurance carriers, administrators, and healthcare providers commonly utilize advanced technology like claims management softwares to automate and digitally manage these claims, streamlining operations and improving overall efficiency.
With this holistic approach, providers can ensure timely processing, accurate billing, and better compliance with insurance-specific regulations.
Key Components of Claims Management
Several key components collectively ensure efficient processing and resolution of insurance claims, typically including:
- Claims submission
- Claims adjudication
- Payment processing
- Denial management
- Claims appeal
Each of these key components in claim management plays a vital role in ensuring a smooth operation and effective processing and resolution of insurance claims.
Below, we’ll delve deeper into each component of claims management distinctly, providing valuable insights to optimize efficiency and accuracy.

Source: freepik.com / Photo Contributor: rawpixel.com
Claims submission
The first key component of claim management is claims submission, in which a provider submits a bill to the patient’s insurance provider detailing the services rendered during their visit. Using current procedural terminology (CPT) codes, healthcare practitioners reflect all the information the insurer needs to know to ensure reimbursement for the covered services. This includes key aspects such as:
- Patient information, including full name, date of birth, and contact details
- The healthcare provider’s National Provider Identifier (NPI)
- CPT codes that detail the provided medical services
To ensure a comprehensive and accurate representation of the provided healthcare services, there are a few practices that can help you along the way. First things first, accurate patient information is one of the key practices for successful claim submission. Ensure that the patient’s data is correct by maintaining regularly updated and accurate patient details in electronic health records (EHRs) to avoid information errors. Next, submit claims within the specified timeframe to reduce the risk of claim denials. Late submissions could lead not only to claim denials, but providers may completely lose the opportunity to receive payment for the services offered.
Claims adjudication
Claims adjudication is a process through which insurance payers review and determine the healthcare claims submitted before reimbursement. Once they receive a claim from providers, insurers carefully review the details before deciding on how they pay the appropriate amount owed for the services rendered (in full or partial amount). Or worse yet, whether they’ll deny the claim. During healthcare claims adjudication in healthcare, insurance payers verify patient eligibility and examine factors such as coverage parameters, and payment policy benefits. If more information is needed, the claim will be rejected with the reason that more documentation is needed in order to be processed.
Payment processing
After the claims adjudication in healthcare, it’s time to process the payment. Payment processing, known as remittance advice or explanation of payment, involves comprehensive audits of the approved payment coverage, the patient’s financial responsibility, and the adjudication date.
Subsequently, the payment is sent to the medical office in the form of either remittance advice or an explanation of payment, contingent on the adjudication decision outcomes. Alongside the financial coverage and credit, providers also receive evaluated and detailed explanations associated with the reasons for their final determination. Typically, this document includes:
- Details on covered and non-covered medical services
- Applied deductibles, co-payments, or co-insurance
- Information on maximum allowable charges or fees
- Clarification on coding discrepancies or modifiers used
- Additional instructions for follow-up or appeal
- Reasons for any claim denials or adjustments
Once the payment is received, it must be accurately posted in the billing system so there isn’t any outstanding balance on the claim.
Denial management
Denial management involves the systematic process of preventing, identifying, analyzing, and resolving claim denials in healthcare billing. It focuses on understanding the reasons behind claim denials and resolving issues promptly while preventing future rejections.
There are numerous reasons why claims may be denied, but the most common include missing or incorrect patient information, coding errors, misspellings, or mistyped numerals. Other frequent causes are incorrect or duplicate claims, lack of medical necessity, expired insurance coverage, and policy limitations that exceed the scope of the patient’s insurance plan.
Claims appeals
Once organizations receive denied medical claims, they must be resolved before the timely filing limit. Insurers have varying policies regarding the appeal, as some allow 90 days for resolutions to be filed while others allow up to a year. Claims appeals refer to the process by which an individual or organization requests a review of a denied or partially denied claim, typically related to insurance or healthcare services.
When a claim is denied, healthcare providers receive an Explanation of Benefits (EOB) detailing the reasons for the denial. Then they are given time to resubmit the claim or file an appeal. During the appeal, the claim gets reviewed, and a decision is made to either uphold the original denial, partially improve the denial, fully reverse the denial, or approve the claim.
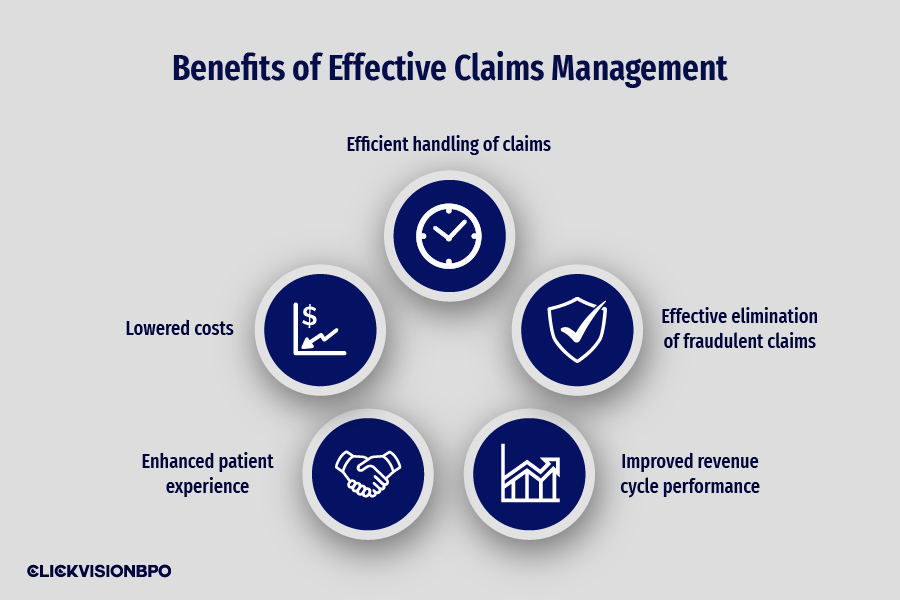
Benefits of Effective Claims Management
Effective claims management is critical for healthcare providers, payers, and patients. With optimized processes in place, organizations can leverage the numerous benefits, including:
- Efficient handling of claims – effective claim management promotes streamlined operations from submission to payment, reducing administrative burdens or delays and ensuring timely processing. This efficiency results in faster reimbursement rates and improved cash flow for providers.
- Effective elimination of fraudulent claims – with the sheer amount of claims submitted, insurers are bound to run into fraudulent claims. However, with a great revenue cycle management strategy in place, you can easily identify and prevent fraudulent claims, protecting financial resources and maintaining integrity altogether.
- Improved revenue cycle performance – optimizing claim submission, adjudication, and payment processes, claim management leads to a healthier revenue cycle, reduced A/R days, reduced claim denials, and increased revenue generation.
- Enhanced patient experience – efficient claim management results in accurate and transparent billing practices, leading to fewer errors and inquiries. This helps facilitate smoother interactions with patients and insurers, resulting in higher satisfaction and experience levels.
- Lowered costs – optimizing claim management can significantly reduce administrative burdens and costs related to resubmissions, errors, and follow-ups on denied claims. With improved operational efficiency, providers can enjoy substantial cost savings.
Conclusion
What is claims management in healthcare? Claim management is the fundamental aspect of healthcare medical billing that encompasses several key components, such as claim submission, adjudication, processing, denial management, and claims appeals. Each component plays a vital role in optimizing revenue cycles and minimizing claim-related issues.
From efficient handling of claims to enhanced patient satisfaction and reduced costs, CLICKVISION BPO can provide complete revenue cycle management services that integrate experience and precision, ultimately contributing to providers’ financial health and operational excellence.

With a strong background in the marketing industry and healthcare leadership roles, Filip is responsible for CLICKVISIONBPO’s sales strategies and onboarding new clients. With a passion for sharing insights gained from his experience, he also shares valuable knowledge through industry related articles.
